
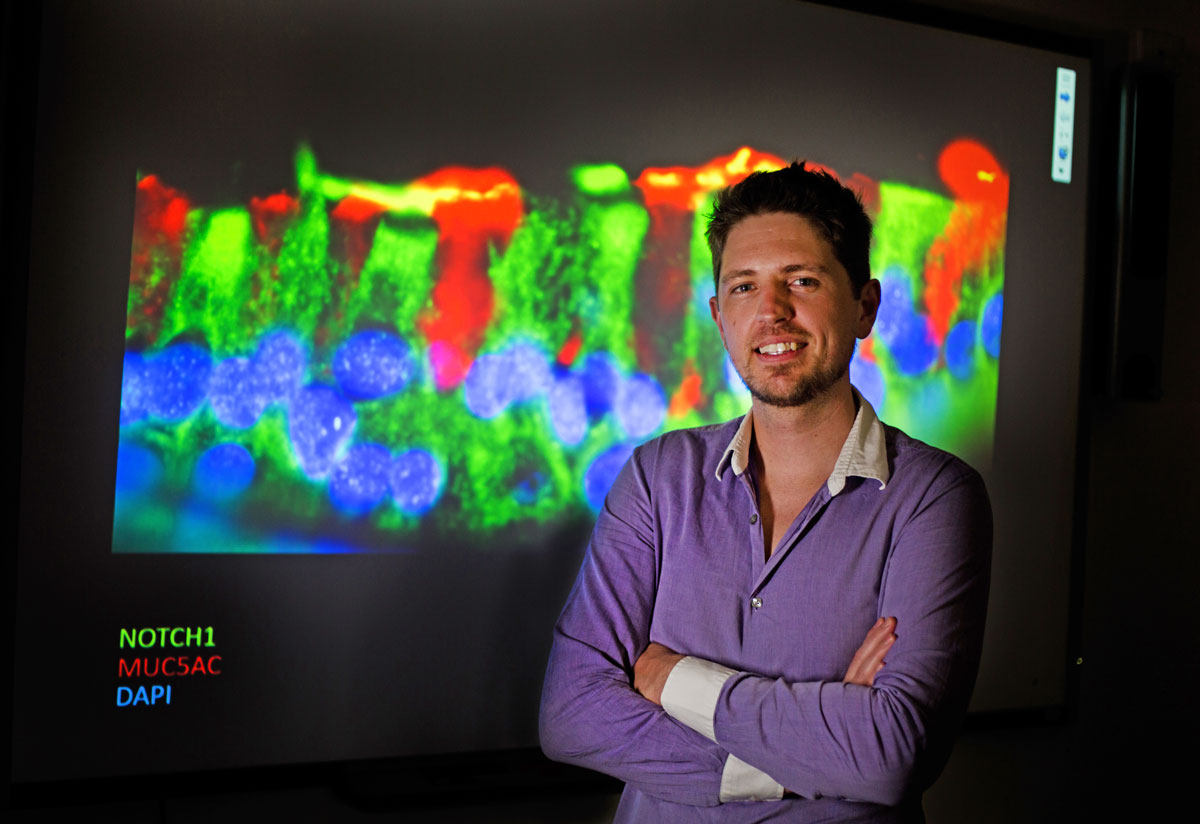
Dr Andrew Reid
Postdoctoral Researcher
School of Medicine and Public Health
- Email:andrew.reid@newcastle.edu.au
- Phone:0240420108
Telescopes to Microscopes: an ingrained love for science
Dr Andrew Reid may have taken the long road to medical research, but it’s not one he regrets.
“When I was still in high school my real passion was astronomy – my Dad had bought me a telescope and I got really into it."
“So when I started out at university, I was doing a double major in maths and physics.”
Hailing from the Central Coast, Andrew’s regular commute to Sydney for his studies was a gruelling one.
“Once I got to the third year it all got to be too much – I ended up deferring and I worked in retail for a while. Then one evening I was talking to my manager – who had always wanted to be a police officer – and we made a deal. He would join the police force and I would go back to university.”
Andrew transferred his credits to UON and was able to complete his science degree, but with a major in biology.
“It turns out biology and chemistry were my calling! I ended up getting First Class Honours and the University Medal.”
On top of those accolades, Andrew was also awarded the Faculty of Science Medal for best thesis and the Barry Boettcher Award for leading grade point average.
For his Honours and PhD projects, Andrew worked in UON’s Reproductive Science group, under the supervision of Dr Shaun Roman and Professor Brett Nixon, respectively.
Andrew’s PhD research focussed on the role of the dynamin protein in sperm maturation and fertilisation. For his work, he was awarded the New Investigator Award from the Australian Society of Reproductive Biology in 2011.
Focus on epithelium
The epithelial cell layer, or ‘epithelium’, occurs throughout the body wherever surfaces come into contact with the outside environment and also on the insides of vessels, tracts and tubules.
The architecture of epithelial cells is highly regulated, and the intracellular junctions are particularly important for maintaining function. These junctions are made up of protein complexes which allow cells to communicate, share nutrients and maintain physical contact with each other.
“The final chapter of my PhD thesis was actually on the epithelium of the epididymis – a duct within the male reproductive system."
“One of the good things about learning about those cells is they stay pretty similar throughout all the different areas of the body.”
Indeed, when Professor Darryl Knight was looking for help in his lab with an asthma research project with the PRC for Healthy Lungs, it turns out Andrew had experience in all the right areas.
“I’ve also got a lot of experience with fluorescence and electron microscopy.”
The disappearing mucus
Previous research by some of Darryl’s international collaborators had highlighted the significance of the Beta-catenin signalling pathway in airway disease, in particular in the epithelial cells lining the airways.
The amount of Beta-catenin protein in the intracellular junctions was different in asthmatic compared to non-asthmatic individuals.
Upon looking closer at this phenomenon, Darryl and Andrew noticed a strange effect of Beta-catenin blocking chemicals.
“Mucus production was decreasing – but it wasn’t via the normal mucus-stimulating cellular pathways. It instead appeared to be happening via the Notch Signalling pathway."
The Notch protein has been well described for its role in tissue development, but this direct involvement in mucus regulation was a novel observation.
Using a specialised cell culture technique, known as air liquid interface culture, researchers within the PRC for Healthy Lungs are able to grow human donor airway epithelial cells in the lab.
The cells differentiate into specific cell types and assume an architecture all but identical to that of the human respiratory epithelial layer.
“Every few days I’ve got to come in and wash off the mucus from the surface of my asthmatic cells and it’s all gluggy and horrible."
“But then when I inhibit Notch, you don’t get that mucus. The cells are all there and they’re happy, they’re still alive - they’re just not spitting out mucus.”
Looking ahead
As well as Notch appearing to regulate mucus production itself, it can also modify the characteristics of the mucus, making it less sticky.
This mucosal stickiness is a problem not just in asthmatics, but also for patients with chronic bronchitis and COPD (Chronic Obstructive Pulmonary Disease).
“We’re hoping to identify which interactions in the Notch signalling pathway are causing these changes in mucus production."
“Then we could design new pharmaceuticals targeting these proteins and increase the quality of life for these patients.”
It’s an exciting field, and one that Andrew’s looking forward to continuing to explore.
Telescopes to Microscopes: an ingrained love for science
Dr Andrew Reid has a hand in increasing the life of asthma patients.
Career Summary
Biography
Research overview
Dr Andrew Reid completed his Bachelor of Science (Hons I) degree in 2009 with a perfect grade point average of 7, earning both the Faculty and University medal. He was offered an Australian Postgraduate Award scholarship as well as the Deputy Vice Chancellor’s award to complete his PhD. Andrew's PhD on the role of dynamin in mouse spermatozoa and the epididymal epithelium earned him 3 high ranking publications on the back of hard work during his PhD tenure. In addition to numerous awards throughout his tenure, Dr Reid was nominated for the PhD medal on the back of his exemplary studies.
In 2014, Andrew began his employment under world-renowned epithelial cell biologist Professor Darryl Knight at the Hunter Medical Research Institute. Here, Andrew's experience in a wide range of microscopy (including immunofluorescent, high frame rate video, phase contrast and electron microscopy) and pharmacological inhibition techniques were essential in achieving a number of highly referenced publications. In 2018, Andrew began his new role under the mentorship of Conjoint Professor Christopher Grainge to investigate the role of mechanical forces at the dysregulated asthmatic airway epithelium. Dr. Reid and Professor Grainge were a tour de force attracting funding from the highly competitive HMRI Cameron family trust, funding pilot data to investigate cells from donors with bronchiectasis, ultimately leading to their successful NHMRC Ideas grant late in 2021.
Collaborations
Dr Reid has encouraged a number of local as well as international collaborations throughout his PhD. And post-doctoral Collaborations. During his PhD, Andrew’s established collaborations with UoN's own Prof. Adam McCluskey (Chemistry) and Prof. Phil Robinson of the Children's Medical Research Institute helped him publish multiple papers on the role of dynamin in fertility. Further collaborations during Dr. Reid’s post-doctoral tenure, with Dr. Benjamin Vaughan (Information and Physical Sciences, UoN), Dr Randy Suryadinata (Royal Children’s Hospital, Melbourne), James Hogg Centre for Heart Lung Innovation (BC, Canada), Cornell University (New York), Prof. Jin-Ah Park (Harvard, MA, USA) and Prof. Aran Singanayagam (Imperial College, London, UK) have enabled a wide network for rare sample attainment and new research ideas and sharing and have led to further funding outcomes.
Qualifications
- Doctor of Philosophy, University of Newcastle
Keywords
- Air-liquid Interface culture
- Airway epithelium
- Asthma
- COPD
- ELISA
- Immunocytochemistry
- Immunohistochemistry
- Molecular biology
- Mucus
- Nanostring
- Notch signalling
- PCR
- Western blotting
- qPCR
Fields of Research
| Code | Description | Percentage |
|---|---|---|
| 320103 | Respiratory diseases | 50 |
| 320801 | Cell physiology | 50 |
Professional Experience
Academic appointment
| Dates | Title | Organisation / Department |
|---|---|---|
| 1/1/2017 - | Postdoctoral Researcher - Respiratory Medicine | College Health, Medicine and Wellbeing - The University of Newcastle (Australia) School of Medicine and Public Health Australia |
Professional appointment
| Dates | Title | Organisation / Department |
|---|---|---|
| 31/1/2014 - 31/12/2017 |
Posdoctoral Researcher During this time I performed experiments using primary bronchial epithelial cells grown at the air-liquid interface from asthmatic and non-asthmatic donors. I also Investigated the Notch and beta-catenin signalling pathways within asthmatic and non-asthmatic airways. I performed pharmacological inhibition of these pathways and analysed the effects on airway morphology. I also developed a number of immunofluorescence and protein quantification techniques used in our laboratory today. |
The University of Newcastle - School of Biomedical Sciences and Pharmacy Respiratory Australia |
Awards
Award
| Year | Award |
|---|---|
| 2010 |
University Medal The University of Newcastle |
| 2010 |
Faculty Medal Faculty of Science and Information Technology,The University of Newcastle |
Prize
| Year | Award |
|---|---|
| 2017 |
Conference Travel Award The Thoracic Society of Australia & New Zealand |
| 2017 |
Cell/Biology/Immunology SIG award The Thoracic Society of Australia and New Zealand |
| 2016 |
Early Career Award Priority Research Centre (PRC) for Healthy Lungs | The University of Newcastle |
| 2013 |
Beautiful Science award The University of Newcastle, School of Biomedical Sciences and Pharmacy |
| 2012 |
Society for Reproductive Biology travel award Australian Society for Reproductive Biology |
| 2011 |
New Investigator Award Australian Society of Reproductive Biology |
| 2011 |
Society for Reproductive Biology travel award Australian Society for Reproductive Biology |
| 2010 |
Barry Boettcher Award Faculty of Science and Information Technology,The University of Newcastle |
| 2010 |
Australian Postgraduate Award The University of Newcastle |
| 2010 |
Deputy Vice Chancellor Research and Innovation Scholarship The University of Newcastle |
Teaching
| Code | Course | Role | Duration |
|---|---|---|---|
| BIOL3090 |
Molecular Biology Faculty of Science and Information Technology, The University of Newcastle | Australia Assessed and marked presentations given by students as per tutorial demonstrator role. |
Head Tutorial Demonstrator | 1/7/2010 - 30/6/2011 |
| BIOL2001 |
Molecular Laboratory Skills for Biological Sciences Faculty of Science and Information Technology, The University of Newcastle | Australia Laboratory Demonstrator |
Laboratory Demonstrator | 2/3/2009 - 30/6/2009 |
| BIOL2001 |
Molecular Laboratory Skills for Biological Sciences Faculty of Science and Information Technology, The University of Newcastle | Australia Head Laboratory Demonstrator |
Laboratory Demonstrator | 1/3/2010 - 30/6/2010 |
Publications
For publications that are currently unpublished or in-press, details are shown in italics.
Chapter (2 outputs)
| Year | Citation | Altmetrics | Link | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 |
Reid AT, Sutanto EN, Chander-Veerati P, Looi K, Li NF, Iosifidis T, Loo S-L, Garratt LW, Kicic A, AusREC , 'Chapter 3 Ground zero—the airway epithelium', 61-98 (2019)
|
||||||||||
| 2019 |
Reid AT, Sutanto EN, Chander-Veerati P, Looi K, Li NF, Iosifidis T, Loo SL, Garratt LW, Kicic A, 'Ground zero-the airway epithelium', 61-98 (2019) [B1]
|
Open Research Newcastle | |||||||||
Conference (22 outputs)
| Year | Citation | Altmetrics | Link | |||||
|---|---|---|---|---|---|---|---|---|
| 2024 |
Reid A, Grainge C, Veerati P, Nichol K, Wark P, 'Airway cells from bronchiectasis patients demonstrate reduced mucociliary clearance in vitro', RESPIROLOGY, 29, 140-140 (2024)
|
|||||||
| 2023 |
Kanwal A, Bartlett NW, Schuliga M, Reid AT, Jackson C, 'Increased IL-25 Expression in Idiopathic Pulmonary Fibrosis and Role in Fibroblast Proliferation and Activation', AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE, 207 (2023)
|
|||||||
| 2021 |
Ngan FL, Reid A, Nichol K, Grainge C, Wark P, Knight D, Bartlett N, 'Dysregulated actin cytoskeleton associated with barrier dysfunction in asthma', FASEB JOURNAL, 35 (2021)
|
|||||||
| 2015 | Moheimani F, Roth H, Cross J, Reid A, Shaheen F, Warner S, Hackett T, Hirota J, Utokaparch S, Kicic A, Hansbro P, Hallstrand T, Kahn M, Stick S, Knight D, 'SUPPRESSION OF beta-CATENIN/CBP SIGNALING INHIBITS EPITHELIAL-MESENCHYMAL TRANSITION AND MIGRATION OF HUMAN AIRWAY EPITHELIUM', RESPIROLOGY, 20, 97-97 (2015) [E3] | |||||||
| 2010 | Reid AT, McEwan K, Campbell DM, Jans DA, Roman SD, 'Consistent nucleosome retention during chromatin packaging in human spermatozoa', OzBio 2010: The Molecules of Life - from Discovery to Biotechnology. Poster Abstracts (2010) [E3] | |||||||
| 2010 |
Reid AT, Roman SD, Aitken RJ, Nixon B, 'Investigation of the role of dynamin in sperm surface remodelling', OzBio 2010: The Molecules of Life - from Discovery to Biotechnology. Poster Abstracts (2010) [E3]
|
|||||||
| 2010 | Roman SD, Reid AT, McEwan K, Campbell DM, Jans DA, 'Nucleosome Retention During Chromatin Packaging in Spermatozoa', Reproduction, Fertility and Development, 22 (2010) [E3] | |||||||
| 2010 |
Reid AT, Roman SD, Aitken RJ, Nixon B, 'Characterisation of the GTPASE dynamin throughout murine sperm maturation', Reproduction, Fertility and Development, 22 (2010) [E3]
|
|||||||
| Show 19 more conferences | ||||||||
Journal article (32 outputs)
| Year | Citation | Altmetrics | Link | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2026 |
Davidson LA, Niessen NM, Rowlandson M, Hibberd AD, Heer MK, Hsu ACY, Kaiko GE, Reid AT, Mayall JR, Horvat JC, Trevillian PR, Baines KJ, 'Mining bulk transcriptomic datasets identifies inflammasome activation and antigen presentation as key novel mechanisms of BK polyomavirus-associated nephropathy', Journal of Pathology, 268, 288-297 (2026)
|
||||||||||
| 2025 |
Chen L, A. Hoefel G, Pathinayake PS, Reid A, Pillar AL, Kelly C, Tan H, Ali A, Kim RY, Hansbro PM, Brody SL, Foster PS, Horvat JC, Riveros C, Awatade N, Wark PAB, Kaiko GE, 'Inflammation-induced loss of CFTR-expressing airway ionocytes in non-eosinophilic asthma', RESPIROLOGY, 30, 25-40 (2025) [C1]
|
||||||||||
| 2024 |
Read J, Reid AT, Thomson C, Plit M, Mejia R, Knight DA, Lize M, El Kasmi K, Grainge CL, Stahl H, Schuliga M, 'Alveolar epithelial cells of lung fibrosis patients are susceptible to severe virus-induced injury', CLINICAL SCIENCE, 138, 537-554 (2024) [C1]
|
Open Research Newcastle | |||||||||
| 2023 |
Veerati PC, Reid AT, Nichol KS, Wark PAB, Knight DA, Bartlett NW, Grainge CL, 'Mechanical forces suppress antiviral innate immune responses from asthmatic airway epithelial cells following rhinovirus infection', AMERICAN JOURNAL OF PHYSIOLOGY-LUNG CELLULAR AND MOLECULAR PHYSIOLOGY, 325, L206-L214 (2023) [C1]
|
Open Research Newcastle | |||||||||
| 2023 |
Awatade NT, Reid AT, Nichol KS, Budden KF, Veerati PC, Pathinayake PS, Grainge CL, Hansbro PM, Wark PAB, 'Comparison of commercially available differentiation media on cell morphology, function, and anti-viral responses in conditionally reprogrammed human bronchial epithelial cells', SCIENTIFIC REPORTS, 13 (2023) [C1]
|
Open Research Newcastle | |||||||||
| 2022 |
Williams TC, Loo S-L, Nichol KS, Reid AT, Veerati PC, Esneau C, Wark PAB, Grainge CL, Knight DA, Vincent T, Jackson CL, Alton K, Shimkets RA, Girkin JL, Bartlett NW, 'IL-25 blockade augments antiviral immunity during respiratory virus infection', COMMUNICATIONS BIOLOGY, 5 (2022) [C1]
|
Open Research Newcastle | |||||||||
| 2022 |
Pathinayake PS, Waters DW, Nichol KS, Brown AC, Reid AT, Hsu AC-Y, Horvat JC, Wood LG, Baines KJ, Simpson JL, Gibson PG, Hansbro PM, Wark PAB, 'Endoplasmic reticulum-unfolded protein response signalling is altered in severe eosinophilic and neutrophilic asthma', THORAX, 77, 443-451 (2022) [C1]
|
Open Research Newcastle | |||||||||
| 2022 |
Veerati PC, Nichol KS, Read JM, Bartlett NW, Wark PAB, Knight DA, Grainge CL, Reid AT, 'Conditionally reprogrammed asthmatic bronchial epithelial cells express lower FOXJ1 at terminal differentiation and lower IFNs following RV-A1 infection', AMERICAN JOURNAL OF PHYSIOLOGY-LUNG CELLULAR AND MOLECULAR PHYSIOLOGY, 323, L495-L502 (2022) [C1]
|
Open Research Newcastle | |||||||||
| 2022 |
Kan S, Grainge C, Nichol K, Reid A, Knight D, Sun Y, Bartlett N, Liang M, 'TLR7 agonist loaded airway epithelial targeting nanoparticles stimulate innate immunity and suppress viral replication in human bronchial epithelial cells', INTERNATIONAL JOURNAL OF PHARMACEUTICS, 617 (2022) [C1]
|
Open Research Newcastle | |||||||||
| 2021 |
Kuchibhotla VNS, Starkey MR, Reid AT, Heijink IH, Nawijn MC, Hansbro PM, Knight DA, 'Inhibition of ß-Catenin/CREB Binding Protein Signaling Attenuates House Dust Mite-Induced Goblet Cell Metaplasia in Mice', FRONTIERS IN PHYSIOLOGY, 12 (2021) [C1]
|
Open Research Newcastle | |||||||||
| 2021 |
Girkin J, Loo S-L, Esneau C, Maltby S, Mercuri F, Chua B, Reid AT, Veerati PC, Grainge CL, Wark PAB, Knight D, Jackson D, Demaison C, Bartlett NW, 'TLR2-mediated innate immune priming boosts lung anti-viral immunity', EUROPEAN RESPIRATORY JOURNAL, 58 (2021) [C1]
|
Open Research Newcastle | |||||||||
| 2021 |
Wark PAB, Pathinayake PS, Kaiko G, Nichol K, Ali A, Chen L, Sutanto EN, Garratt LW, Sohal SS, Lu W, Eapen MS, Oldmeadow C, Bartlett N, Reid A, Veerati P, Hsu AC-Y, Looi K, Iosifidis T, Stick SM, Hansbro PM, Kicic A, 'ACE2 expression is elevated in airway epithelial cells from older and male healthy individuals but reduced in asthma', RESPIROLOGY, 26, 442-451 (2021) [C1]
Background and objective: COVID-19 is complicated by acute lung injury, and death in some individuals. It is caused by SARS-CoV-2 that requires the ACE2 receptor and se... [more] Background and objective: COVID-19 is complicated by acute lung injury, and death in some individuals. It is caused by SARS-CoV-2 that requires the ACE2 receptor and serine proteases to enter AEC. We determined what factors are associated with ACE2 expression particularly in patients with asthma and COPD. Methods: We obtained lower AEC from 145 people from two independent cohorts, aged 2¿89 years, Newcastle (n = 115) and Perth (n = 30), Australia. The Newcastle cohort was enriched with people with asthma (n = 37) and COPD (n = 38). Gene expression for ACE2 and other genes potentially associated with SARS-CoV-2 cell entry was assessed by qPCR, and protein expression was confirmed with immunohistochemistry on endobronchial biopsies and cultured AEC. Results: Increased gene expression of ACE2 was associated with older age (P = 0.03) and male sex (P = 0.03), but not with pack-years smoked. When we compared gene expression between adults with asthma, COPD and healthy controls, mean ACE2 expression was lower in asthma patients (P = 0.01). Gene expression of furin, a protease that facilitates viral endocytosis, was also lower in patients with asthma (P = 0.02), while ADAM-17, a disintegrin that cleaves ACE2 from the surface, was increased (P = 0.02). ACE2 protein expression was also reduced in endobronchial biopsies from asthma patients. Conclusion: Increased ACE2 expression occurs in older people and males. Asthma patients have reduced expression. Altered ACE2 expression in the lower airway may be an important factor in virus tropism and may in part explain susceptibility factors and why asthma patients are not over-represented in those with COVID-19 complications.
|
Open Research Newcastle | |||||||||
| 2020 |
Baines KJ, Fricker M, McDonald VM, Simpson JL, Wood LG, Wark PAB, Macdonald HE, Reid A, Gibson PG, 'Sputum transcriptomics implicates increased p38 signalling activity in severe asthma', RESPIROLOGY, 25, 709-718 (2020) [C1]
Background and objective: Severe asthma is responsible for a disproportionate burden of illness and healthcare costs spent on asthma. This study analyses sputum transcr... [more] Background and objective: Severe asthma is responsible for a disproportionate burden of illness and healthcare costs spent on asthma. This study analyses sputum transcriptomics to investigate the mechanisms and novel treatment targets of severe asthma. Methods: Induced sputum samples were collected in a cross-sectional study from participants with severe asthma (n = 12, defined as per GINA criteria), non-severe uncontrolled (n = 21) and controlled asthma (n = 21) and healthy controls (n = 15). Sputum RNA was extracted and transcriptomic profiles were generated (Illumina HumanRef-8 V2) and analysed (GeneSpring). Sputum protein lysates were analysed for p38 activation in a validation study (n = 24 asthma, n = 8 healthy) by western blotting. Results: There were 2166 genes differentially expressed between the four groups. In severe asthma, the expression of 1875, 1308 and 563 genes was altered compared to healthy controls, controlled and uncontrolled asthma, respectively. Of the 1875 genes significantly different to healthy controls, 123 were >2-fold change from which four networks were identified. Thirty genes (>2-fold change) were significantly different in severe asthma compared to both controlled asthma and healthy controls. There was enrichment of genes in the p38 signalling pathway that were associated with severe asthma. Phosphorylation of p38 was increased in a subset of severe asthma samples, correlating with neutrophilic airway inflammation. Conclusion: Severe asthma is associated with substantial differences in sputum gene expression that underlie unique cellular mechanisms. The p38 signalling pathway may be important in the pathogenesis of severe asthma, and future investigations into p38 inhibition are warranted as a 'non-Th2' therapeutic option.
|
Open Research Newcastle | |||||||||
| 2020 |
Schuliga M, Read J, Blokland KEC, Waters DW, Burgess J, Prele C, Mutsaers SE, Jaffar J, Westall G, Reid A, James A, Grainge C, Knight DA, 'Self DNA perpetuates IPF lung fibroblast senescence in a cGAS-dependent manner', CLINICAL SCIENCE, 134, 889-905 (2020) [C1]
|
Open Research Newcastle | |||||||||
| 2020 |
Veerati PC, Mitchel JA, Reid AT, Knight DA, Bartlett NW, Park JA, Grainge CL, 'Airway mechanical compression: Its role in asthma pathogenesis and progression', European Respiratory Review, 29, 1-13 (2020) [C1]
|
Open Research Newcastle | |||||||||
| 2020 |
Kicic A, de Jong E, Ling K-M, Nichol K, Anderson D, Wark PAB, Knight DA, Bosco A, Stick SM, 'Assessing the unified airway hypothesis in children via transcriptional profiling of the airway epithelium', JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY, 145, 1562-1573 (2020) [C1]
|
Open Research Newcastle | |||||||||
| 2020 |
Reid AT, Nichol KS, Veerati PC, Moheimani F, Kicic A, Stick SM, Bartlett NW, Grainge CL, Wark PAB, Hansbro PM, Knight DA, 'Blocking Notch3 Signaling Abolishes MUC5AC Production in Airway Epithelial Cells from Individuals with Asthma', AMERICAN JOURNAL OF RESPIRATORY CELL AND MOLECULAR BIOLOGY, 62, 513-523 (2020) [C1]
In asthma, goblet cell numbers are increased within the airway epithelium, perpetuating the production of mucus that is more difficult to clear and results in airway mu... [more] In asthma, goblet cell numbers are increased within the airway epithelium, perpetuating the production of mucus that is more difficult to clear and results in airway mucus plugging. Notch1, Notch2, or Notch3, or a combination of these has been shown to influence the differentiation of airway epithelial cells. How the expression of specific Notch isoforms differs in fully differentiated adult asthmatic epithelium and whether Notch influences mucin production after differentiation is currently unknown. We aimed to quantify different Notch isoforms in the airway epithelium of individuals with severe asthma and to examine the impact of Notch signaling on mucin MUC5AC. Human lung sections and primary bronchial epithelial cells from individuals with and without asthma were used in this study. Primary bronchial epithelial cells were differentiated at the air-liquid interface for 28 days. Notch isoform expression was analyzed by Taqman quantitative PCR. Immunohistochemistry was used to localize and quantify Notch isoforms in human airway sections. Notch signaling was inhibited in vitro using dibenzazepine or Notch3-specific siRNA, followed by analysis of MUC5AC. NOTCH3 was highly expressed in asthmatic airway epithelium compared with nonasthmatic epithelium. Dibenzazepine significantly reduced MUC5AC production in air-liquid interface cultures of primary bronchial epithelial cells concomitantly with suppression of NOTCH3 intracellular domain protein. Specific knockdown using NOTCH3 siRNA recapitulated the dibenzazepine-induced reduction in MUC5AC. We demonstrate that NOTCH3 is a regulator of MUC5AC production. Increased NOTCH3 signaling in the asthmatic airway epithelium may therefore be an underlying driver of excess MUC5AC production.
|
Open Research Newcastle | |||||||||
| 2020 |
Veerati PC, Troy NM, Reid AT, Li NF, Nichol KS, Kaur P, Maltby S, Wark PAB, Knight DA, Bosco A, Grainge CL, Bartlett NW, 'Airway Epithelial Cell Immunity Is Delayed During Rhinovirus Infection in Asthma and COPD', FRONTIERS IN IMMUNOLOGY, 11 (2020) [C1]
|
Open Research Newcastle | |||||||||
| 2019 |
Nalesso E, Hearn A, Sosa-Nishizaki O, Steiner T, Antoniou A, Reid A, Bessudo S, Soler G, Klimley P, Lara F, Ketchum JT, Arauz R, 'Movements of scalloped hammerhead sharks (Sphyrna lewini) at Cocos Island, Costa Rica and between oceanic islands in the Eastern Tropical Pacific', PLOS ONE, 14 (2019) [C1]
|
||||||||||
| 2019 |
Singanayagam A, Loo S-L, Calderazzo M, Finney LJ, Torralbo M-BT, Bakhsoliani E, Girkin J, Veerati P, Pathinayake PS, Nichol KS, Reid A, Footitt J, Wark PAB, Grainge CL, Johnston SL, Bartlett NW, Mallia P, 'Antiviral immunity is impaired in COPD patients with frequent exacerbations', AMERICAN JOURNAL OF PHYSIOLOGY-LUNG CELLULAR AND MOLECULAR PHYSIOLOGY, 317, L893-L903 (2019) [C1]
Patients with frequent exacerbations represent a chronic obstructive pulmonary disease (COPD) subgroup requiring better treatment options. The aim of this study was to ... [more] Patients with frequent exacerbations represent a chronic obstructive pulmonary disease (COPD) subgroup requiring better treatment options. The aim of this study was to determine the innate immune mechanisms that underlie susceptibility to frequent exacerbations in COPD. We measured sputum expression of immune mediators and bacterial loads in samples from patients with COPD at stable state and during virusassociated exacerbations. In vitro immune responses to rhinovirus infection in differentiated primary bronchial epithelial cells (BECs) sampled from patients with COPD were additionally evaluated. Patients were stratified as frequent exacerbators (=2 exacerbations in the preceding year) or infrequent exacerbators (<2 exacerbations in the preceding year) with comparisons made between these groups. Frequent exacerbators had reduced sputum cell mRNA expression of the antiviral immune mediators type I and III interferons and reduced interferon-stimulated gene (ISG) expression when clinically stable and during virus-associated exacerbation. A role for epithelial cellintrinsic innate immune dysregulation was identified: induction of interferons and ISGs during in vitro rhinovirus (RV) infection was also impaired in differentiated BECs from frequent exacerbators. Frequent exacerbators additionally had increased sputum bacterial loads at 2 wk following virus-associated exacerbation onset. These data implicate deficient airway innate immunity involving epithelial cells in the increased propensity to exacerbations observed in some patients with COPD. Therapeutic approaches to boost innate antimicrobial immunity in the lung could be a viable strategy for prevention and treatment of frequent exacerbations.
|
Open Research Newcastle | |||||||||
| 2018 |
Reid AT, Veerati PC, Gosens R, Bartlett NW, Wark PA, Grainge CL, Stick SM, Kicic A, Moheimani F, Hansbro PM, Knight DA, 'Persistent induction of goblet cell differentiation in the airways: Therapeutic approaches', PHARMACOLOGY & THERAPEUTICS, 185, 155-169 (2018) [C1]
Dysregulated induction of goblet cell differentiation results in excessive production and retention of mucus and is a common feature of several chronic airways diseases... [more] Dysregulated induction of goblet cell differentiation results in excessive production and retention of mucus and is a common feature of several chronic airways diseases. To date, therapeutic strategies to reduce mucus accumulation have focused primarily on altering the properties of the mucus itself, or have aimed to limit the production of mucus-stimulating cytokines. Here we review the current knowledge of key molecular pathways that are dysregulated during persistent goblet cell differentiation and highlights both pre-existing and novel therapeutic strategies to combat this pathology.
|
Open Research Newcastle | |||||||||
| 2018 |
Schuliga M, Pechkovsky DV, Read J, Waters DW, Blokland KEC, Reid AT, Hogaboam CM, Khalil N, Burgess JK, Prele CM, Mutsaers SE, Jaffar J, Westall G, Grainge C, Knight DA, 'Mitochondrial dysfunction contributes to the senescent phenotype of IPF lung fibroblasts', JOURNAL OF CELLULAR AND MOLECULAR MEDICINE, 22, 5847-5861 (2018) [C1]
|
Open Research Newcastle | |||||||||
| 2018 |
Singanayagam A, Glanville N, Girkin JL, Ching YM, Marcellini A, Porter JD, Toussaint M, Walton RP, Finney LJ, Aniscenko J, Zhu J, Trujillo-Torralbo M-B, Calderazzo MA, Grainge C, Loo S-L, Veerati PC, Pathinayake PS, Nichol KS, Reid AT, James PL, Solari R, Wark PAB, Knight DA, Moffatt MF, Cookson WO, Edwards MR, Mallia P, Bartlett NW, Johnston SL, 'Corticosteroid suppression of antiviral immunity increases bacterial loads and mucus production in COPD exacerbations', NATURE COMMUNICATIONS, 9 (2018) [C1]
|
Open Research Newcastle | |||||||||
| 2018 |
Moheimani F, Koops J, Williams T, Reid AT, Hansbro PM, Wark PA, Knight DA, 'Influenza A virus infection dysregulates the expression of microRNA-22 and its targets; CD147 and HDAC4, in epithelium of asthmatics', Respiratory Research, 19 (2018) [C1]
|
Open Research Newcastle | |||||||||
| 2017 |
Zhou W, De Iuliis GN, Turner AP, Reid AT, Anderson AL, McCluskey A, McLaughlin EA, Nixon B, 'Developmental expression of the dynamin family of mechanoenzymes in the mouse epididymis', BIOLOGY OF REPRODUCTION, 96, 159-173 (2017) [C1]
|
Open Research Newcastle | |||||||||
| 2016 |
Moheimani F, Hsu AC-Y, Reid AT, Williams T, Kicic A, Stick SM, Hansbro PM, Wark PAB, Knight DA, 'The genetic and epigenetic landscapes of the epithelium in asthma', RESPIRATORY RESEARCH, 17 (2016) [C1]
|
Open Research Newcastle | |||||||||
| 2015 |
Moheimani F, Roth HM, Cross J, Reid AT, Shaheen F, Warner SM, Hirota JA, Kicic A, Hallstrand TS, Kahn M, Stick SM, Hansbro PM, Hackett T-L, Knight DA, 'Disruption of ß-catenin/CBP signaling inhibits human airway epithelial-mesenchymal transition and repair', INTERNATIONAL JOURNAL OF BIOCHEMISTRY & CELL BIOLOGY, 68, 59-69 (2015) [C1]
The epithelium of asthmatics is characterized by reduced expression of E-cadherin and increased expression of the basal cell markers ck-5 and p63 that is indicative of ... [more] The epithelium of asthmatics is characterized by reduced expression of E-cadherin and increased expression of the basal cell markers ck-5 and p63 that is indicative of a relatively undifferentiated repairing epithelium. This phenotype correlates with increased proliferation, compromised wound healing and an enhanced capacity to undergo epithelial-mesenchymal transition (EMT). The transcription factor ß-catenin plays a vital role in epithelial cell differentiation and regeneration, depending on the co-factor recruited. Transcriptional programs driven by the ß-catenin/CBP axis are critical for maintaining an undifferentiated and proliferative state, whereas the ß-catenin/p300 axis is associated with cell differentiation. We hypothesized that disrupting the ß-catenin/CBP signaling axis would promote epithelial differentiation and inhibit EMT. We treated monolayer cultures of human airway epithelial cells with TGFß1 in the presence or absence of the selective small molecule ICG-001 to inhibit ß-catenin/CBP signaling. We used western blots to assess expression of an EMT signature, CBP, p300, ß-catenin, fibronectin and ITGß1 and scratch wound assays to assess epithelial cell migration. Snai-1 and -2 expressions were determined using q-PCR. Exposure to TGFß1 induced EMT, characterized by reduced E-cadherin expression with increased expression of a-smooth muscle actin and EDA-fibronectin. Either co-treatment or therapeutic administration of ICG-001 completely inhibited TGFß1-induced EMT. ICG-001 also reduced the expression of ck-5 and -19 independent of TGFß1. Exposure to ICG-001 significantly inhibited epithelial cell proliferation and migration, coincident with a down regulation of ITGß1 and fibronectin expression. These data support our hypothesis that modulating the ß-catenin/CBP signaling axis plays a key role in epithelial plasticity and function.
|
Open Research Newcastle | |||||||||
| 2015 |
Reid AT, Anderson AL, Roman SD, McLaughlin EA, McCluskey A, Robinson PJ, Aitken RJ, Nixon B, 'Glycogen synthase kinase 3 regulates acrosomal exocytosis in mouse spermatozoa via dynamin phosphorylation', FASEB JOURNAL, 29, 2872-2882 (2015) [C1]
|
Open Research Newcastle | |||||||||
| 2012 |
Reid AT, Lord T, Stanger SJ, Roman SD, McCluskey A, Robinson PJ, Aitken RJ, Nixon B, 'Dynamin regulates specific membrane fusion events necessary for acrosomal exocytosis in mouse spermatozoa', Journal of Biological Chemistry, 287, 37659-37672 (2012) [C1]
|
Open Research Newcastle | |||||||||
| 2010 |
Reid AT, Redgrove KA, Aitken RJ, Nixon B, 'Cellular mechanisms regulating sperm-zona pellucida interaction', Asian Journal of Andrology, 13, 88-96 (2010) [C1]
|
||||||||||
| Show 29 more journal articles | |||||||||||
Preprint (6 outputs)
| Year | Citation | Altmetrics | Link | |||||
|---|---|---|---|---|---|---|---|---|
| 2023 |
Awatade N, Reid A, Nichol K, Budden K, Veerati P, Pathinayake P, Grainge C, Hansbro P, Wark PAB, 'Comparison of commercially available differentiation media on morphology, function, and virus-host interaction in conditionally reprogrammed human bronchial epithelial cells' (2023)
|
|||||||
| 2023 |
Awatade NT, Reid AT, Nichol KS, Budden KF, Veerati PC, Pathinayake PS, Grainge CL, Hansbro PM, Wark PAB, 'Comparison of Commercially Available Differentiation Media on Cell Morphology, Function, and Anti-Viral Responses in Conditionally Reprogrammed Human Bronchial Epithelial Cells' (2023)
|
|||||||
| 2022 |
Chen L, Hoefel GA, Pathinayake P, Reid A, Kelly C, HuiYing T, Kim R, Hansbro P, Brody S, Foster P, Horvat J, Riveros C, Wark PAB, Kaiko G, 'Single cell RNA-seq identifies inflammation-induced loss of CFTR-expressing airway ionocytes in non-eosinophilic asthma' (2022)
|
|||||||
| Show 3 more preprints | ||||||||
Grants and Funding
Summary
| Number of grants | 13 |
|---|---|
| Total funding | $1,193,396 |
Click on a grant title below to expand the full details for that specific grant.
20251 grants / $16,226
Mapping the signalling pathways in lung tissue from donors with bronchiectasis using spatial transcriptomics$16,226
Funding body: Hunter New England Local Health District
| Funding body | Hunter New England Local Health District |
|---|---|
| Project Team | Dr Andrew Reid, Felicia Ton |
| Scheme | John Hunter Hospital Charitable Trust Grant |
| Role | Lead |
| Funding Start | 2025 |
| Funding Finish | 2025 |
| GNo | G2501201 |
| Type Of Funding | C2300 – Aust StateTerritoryLocal – Own Purpose |
| Category | 2300 |
| UON | Y |
20243 grants / $58,914
Development of patient-centric drug screening platform to address deficient mucociliary clearance in PCD$30,000
Funding body: Lung Foundation Australia
| Funding body | Lung Foundation Australia |
|---|---|
| Project Team | Dr Andrew Reid, Conj Assoc Prof Christopher Grainge, Conj Assoc Prof Christopher Grainge, Professor Peter Wark, Con Prof Peter Wark |
| Scheme | PCD Australia Fellowship |
| Role | Lead |
| Funding Start | 2024 |
| Funding Finish | 2026 |
| GNo | G2301142 |
| Type Of Funding | C3200 – Aust Not-for Profit |
| Category | 3200 |
| UON | Y |
Are areas of observable bronchiectasis pathology functionally unique to normal areas of the lung in the same patient?$18,430
Funding body: Hunter New England Local Health District
| Funding body | Hunter New England Local Health District |
|---|---|
| Project Team | Dr Andrew Reid, Felicia Ton |
| Scheme | John Hunter Hospital Charitable Trust Grant |
| Role | Lead |
| Funding Start | 2024 |
| Funding Finish | 2024 |
| GNo | G2400572 |
| Type Of Funding | C2300 – Aust StateTerritoryLocal – Own Purpose |
| Category | 2300 |
| UON | Y |
Smarter Therapeutic and Diagnostic Intervention in Malignant Pleural Effusion: A feasibility randomised trial$10,484
Funding body: Hunter New England Local Health District
| Funding body | Hunter New England Local Health District |
|---|---|
| Project Team | Dr Vineeth George, Conj Assoc Prof Christopher Grainge, Dr Andrew Reid |
| Scheme | John Hunter Hospital Charitable Trust Grant |
| Role | Investigator |
| Funding Start | 2024 |
| Funding Finish | 2024 |
| GNo | G2301359 |
| Type Of Funding | C2300 – Aust StateTerritoryLocal – Own Purpose |
| Category | 2300 |
| UON | Y |
20231 grants / $4,783
Primary ciliary dyskinesia mutation frequency in Australians with bronchiectasis - pilot$4,783
Funding body: University of Newcastle
| Funding body | University of Newcastle |
|---|---|
| Project Team | Dr Andrew Reid |
| Scheme | Pilot Funding Scheme |
| Role | Lead |
| Funding Start | 2023 |
| Funding Finish | 2023 |
| GNo | G2300449 |
| Type Of Funding | Internal |
| Category | INTE |
| UON | Y |
20221 grants / $946,962
Impaired mucociliary clearance drives Bronchiectasis progression$946,962
Funding body: NHMRC (National Health & Medical Research Council)
| Funding body | NHMRC (National Health & Medical Research Council) |
|---|---|
| Project Team | Conj Assoc Prof Christopher Grainge, Dr Andrew Reid, Alan Hsu, Dr Punnam Chander Veerati, Dr Alan Hsu |
| Scheme | Ideas Grants |
| Role | Investigator |
| Funding Start | 2022 |
| Funding Finish | 2025 |
| GNo | G2100438 |
| Type Of Funding | C1100 - Aust Competitive - NHMRC |
| Category | 1100 |
| UON | Y |
20191 grants / $50,407
The role of apical mechanical shear stress on epithelial cell function in asthma$50,407
Funding body: Hunter New England Local Health District
| Funding body | Hunter New England Local Health District |
|---|---|
| Project Team | Dr Andrew Reid, Dr Punnam Chander Veerati, Conj Assoc Prof Christopher Grainge, Conj Assoc Prof Christopher Grainge |
| Scheme | John Hunter Hospital Charitable Trust Grant |
| Role | Lead |
| Funding Start | 2019 |
| Funding Finish | 2021 |
| GNo | G1900261 |
| Type Of Funding | C2400 – Aust StateTerritoryLocal – Other |
| Category | 2400 |
| UON | Y |
20182 grants / $39,699
Establishing a comprehensive in vitro model of bronchiectasis$22,893
Funding body: Hunter Medical Research Institute
| Funding body | Hunter Medical Research Institute |
|---|---|
| Project Team | Conj Assoc Prof Christopher Grainge, Dr Andrew Reid, Con Prof Peter Wark, Assoc Prof Katie Baines, Dr Benjamin Vaughan, Dr Punnam Chander Veerati |
| Scheme | Research Grant |
| Role | Investigator |
| Funding Start | 2018 |
| Funding Finish | 2025 |
| GNo | G1901576 |
| Type Of Funding | C3300 – Aust Philanthropy |
| Category | 3300 |
| UON | Y |
The role of apical mechanical shear stress on epithelial cell function in asthma$16,806
Funding body: Hunter Medical Research Institute
| Funding body | Hunter Medical Research Institute |
|---|---|
| Project Team | Dr Andrew Reid, Dr Punnam Chander Veerati, Conj Assoc Prof Christopher Grainge |
| Scheme | Project Grant |
| Role | Lead |
| Funding Start | 2018 |
| Funding Finish | 2022 |
| GNo | G1800434 |
| Type Of Funding | C3200 – Aust Not-for Profit |
| Category | 3200 |
| UON | Y |
20173 grants / $58,420
Zeiss ApoTome.2 Optical Slider assembly$31,458
Funding body: The University of Newcastle
| Funding body | The University of Newcastle |
|---|---|
| Project Team | Foster, P.S., Knight, D.A., Kim, R.Y., Horvat J.C., Bartlett, N.W., Yang, M., Donovan, C., Starkey, M.R., Reid, A.T., Tay, H.L., Kaiko, G., Collison, A.M. |
| Scheme | UON 2017 Researcher Equipment Grant |
| Role | Investigator |
| Funding Start | 2017 |
| Funding Finish | 2017 |
| GNo | |
| Type Of Funding | Internal |
| Category | INTE |
| UON | N |
Hunter Medical Research Institute Equipment Grant$19,198
Funding body: Hunter Medical Research Institute (HMRI)
| Funding body | Hunter Medical Research Institute (HMRI) |
|---|---|
| Project Team | D.A. Knight, N.W. Bartlett, C.L. Grainge, M. Schuliga, M.T. Liang, A.T. Reid |
| Scheme | HMRI Equipment Grant |
| Role | Investigator |
| Funding Start | 2017 |
| Funding Finish | 2017 |
| GNo | |
| Type Of Funding | Internal |
| Category | INTE |
| UON | N |
Development of a medium throughput assay for assessing compounds that modulate fibroblast function in COPD$7,764
Funding body: Metera Pharmaceuticals Inc
| Funding body | Metera Pharmaceuticals Inc |
|---|---|
| Project Team | Professor Darryl Knight, Dr Michael Schuliga, Dr Andrew Reid |
| Scheme | Research Consultancy |
| Role | Investigator |
| Funding Start | 2017 |
| Funding Finish | 2017 |
| GNo | G1701512 |
| Type Of Funding | C3500 – International Not-for profit |
| Category | 3500 |
| UON | Y |
20161 grants / $17,985
Upgrades for existing Zeiss Automated Fluorescent Microscope$17,985
Funding body: The University of Newcastle
| Funding body | The University of Newcastle |
|---|---|
| Project Team | Starkey, M.R., Donovan, C., Kim, R.Y., Reid, A.T., Tay, H.L. |
| Scheme | UoN Researcher Equipment Grant 2016 |
| Role | Investigator |
| Funding Start | 2016 |
| Funding Finish | 2016 |
| GNo | |
| Type Of Funding | Internal |
| Category | INTE |
| UON | N |
Research Supervision
Number of supervisions
Current Supervision
| Commenced | Level of Study | Research Title | Program | Supervisor Type |
|---|---|---|---|---|
| 2022 | PhD | The Role Of Epithelial Senescence In Lung Injury And Fibrosis | PhD (Medical Biochemistry), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2017 | PhD | An Investigation of Regional Heterogeneity of the Pulmonary Microenvironment in Idiopathic Pulmonary Fibrosis | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Consultant Supervisor |
Past Supervision
| Year | Level of Study | Research Title | Program | Supervisor Type |
|---|---|---|---|---|
| 2023 | PhD | The Fibrogenic Actions of IL-25 in Idiopathic Pulmonary Fibrosis (IPF) | PhD (Immunology & Microbiol), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2022 | PhD | The Role of STATs in the Interaction of Virus and Type 2 Cytokines in Airway Epithelial Cells | PhD (Medical Biochemistry), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2021 | PhD | The Role of E-Cadherin/¿-Catenin Signalling in the Development of an Asthmatic Airway Epithelial Phenotype | PhD (Immunology & Microbiol), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2019 | PhD | Role of Mechanical Forces in Asthma Pathogenesis | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
Dr Andrew Reid
Position
Postdoctoral Researcher
Grainge group
School of Medicine and Public Health
College of Health, Medicine and Wellbeing
Contact Details
| andrew.reid@newcastle.edu.au | |
| Phone | 0240420108 |
| Link | Research Networks |
Office
| Room | HMRI2109 |
|---|---|
| Building | Hunter Medical Research Institute |
| Location | John Hunter Hospital Site , |




