Medical training technology
We are developing a diverse range of medical training technologies, encompassing both synthetic training materials and advanced digital platforms that leverage augmented reality (AR) and virtual reality (VR).
A key area of focus is the integration of biofeedback-enabled systems to enhance the effectiveness and interactivity of training experiences.
Our Capabilities
Our team uses laser scanning to make detailed 3D copies of real objects, body parts, and machine parts. These scans can be used to build digital models, study how things work, or add to virtual worlds.
We also use 3D resin printers, mainly with a method called stereolithography, to make high-quality physical models. These models are useful for things like practicing surgery, testing new devices, or checking how parts hold up under stress.
We do many types of mechanical testing, such as pulling, squeezing, bending, and repeated use tests. This helps us understand how materials and parts behave, especially when they are meant to act like human tissue or need to meet certain performance standards.
Our team also works with augmented and virtual reality (AR/VR). We build interactive digital spaces for training, practice, and learning.
We design training systems too, helping create programs that match learning goals and skill levels. These programs often combine hands-on tools with digital ones for education or job training.
Example Projects
TACTICS VR – Immersive Stroke Training for Clinicians
TACTICS VR is a virtual reality training tool that helps doctors learn how to treat stroke patients, especially in rural and regional areas. It uses realistic, hands-on simulations where users practice steps like checking symptoms, doing scans, working with remote stroke experts, and making treatment choices—all in a fast-paced, high-pressure setting.
The tool was created as part of the TACTICS research project and is based on real medical guidelines. It runs on VR headsets and gives users instant feedback, performance scores, and helpful tips.
TACTICS VR is already being used in hospitals across Australia. It helps doctors feel more confident and better prepared to care for stroke patients. The program is now being updated so it can be used in other countries too.

3D-Printed Models for Surgical Training
This project uses CT and MRI imaging data to develop anatomically accurate 3D-printed models for surgical training. Knee MRI Images from the NewRun study have been provided to support model development. The models aim to improve the realism of surgical simulations and enhance trainee skills using imaging-based anatomical structures.
Currently, we are working in partnership with the Hunter New England Local Health District to produce highly realistic materials for surgical training. This includes models that replicate the biomechanics and response properties of human materials. Key partners include: Professor Rohan Walker, Lead of the University of Newcastle's Surgical Skills Training Unit, Dr Matt Farrow, Senior Anatomy Lead, Professor Zsolt Balough, Head of Trauma Surgery; Mr Ishaque Khan, Head of Biomedical Engineering, HNELHD; Associate Professor Yuen Yong, Mechanical Engineering, Professor Sarah Johnson, Electrical Engineering.
Current student investigators: Julian Zulumovski (Biomed Sci); Paris Alford (Mech Eng) Amelia Comley (Mech Eng); Jemma Miyashita (Biomed Sci); Caitlin Goldfinch (Biomed Sci) and Jeziah Watts (Biomed Sci).
Project lead: Prof Rohan Walker
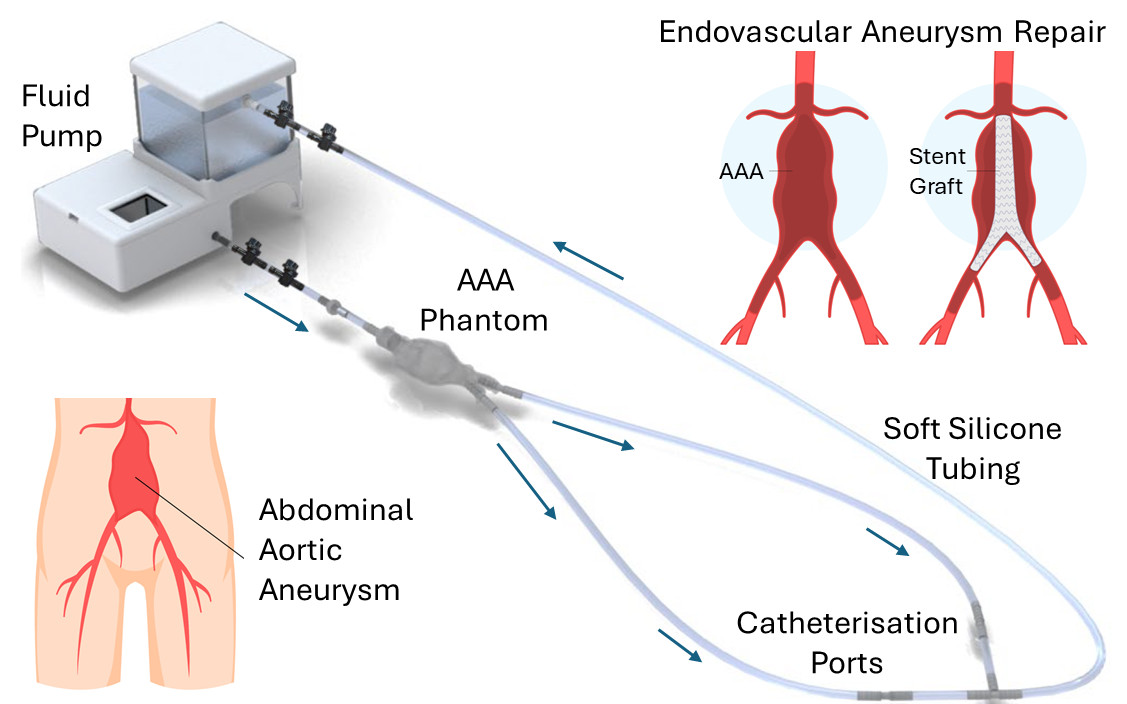
An Abdominal Aorta Aneurysm Simulator for Surgical Training
This project develops a patient-specific Abdominal Aortic Aneurysm (AAA) simulator to enhance training in endovascular aneurysm repair (EVAR). The AAA phantom is fabricated from silicone using CT scan data. A closed-loop hydraulic system that circulates a blood-like fluid is implemented to control fluid pressure and flow, enabling realistic simulation of patient-specific physiological conditions. By improving trainees’ understanding of AAA pathology and EVAR techniques, the simulator aims to reduce reintervention rates and support better long-term outcomes.
Project lead: A/Prof Yuen Yong
Collaborators
- Clinical centres: John Hunter Hospital, Hunter and Central Coast Living Labs
- Industry collaborations: Agency for Clinical Innovation; Smith & Nephew.
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.