Think you’re gluten intolerant? Perhaps think again
Researchers from the University of Newcastle (UON) have highlighted the potential risks of following a gluten-free diet, urging the community to only drastically change their eating habits if formally diagnosed with coeliac disease.
Led by Dr Michael Potter from the Hunter Medical Research Institute, a new narrative review published in the Medical Journal of Australia stresses the adverse effects of changing to a gluten-free diet in light of a self-diagnosis.
Aside from being more expensive and often challenging in a social setting, there is evidence a gluten-free diet can adversely affect human health.
“Several studies have demonstrated that gluten-free diets may not provide adequate amounts of trace elements and vitamins such as calcium and vitamin D.
“A gluten free diet may adversely affect cardiovascular risk factors such as total cholesterol levels, weight gain leading to obesity, glucose intolerance and blood pressure,” the authors wrote.
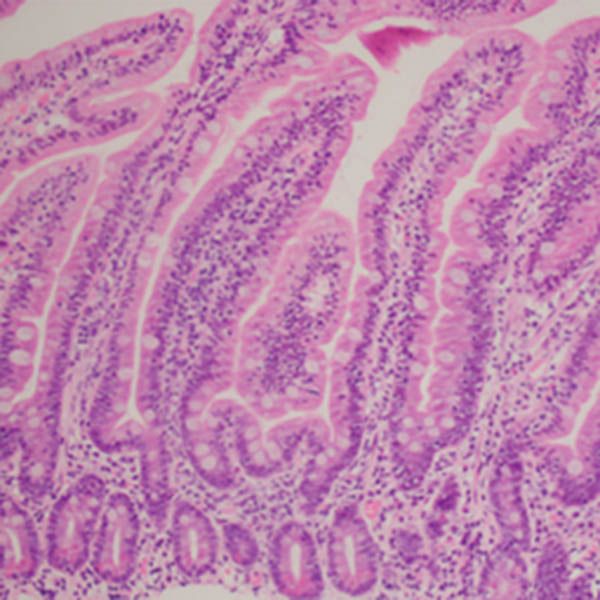
Once considered a rare condition, coeliac disease is now believed to affect up to one in 100 Australians. Despite this, many more Australians report adverse symptoms after eating wheat products and are understood to monitor or limit their gluten intake.
“There are likely to be many in the community who incorrectly attribute adverse physiological symptoms to wheat ingestion and unnecessarily subject themselves to a gluten-free diet,” the authors wrote.
“Gluten may not be wholly responsible for the condition and non-coeliac gluten or wheat sensitivity (NCG/WS) could be a more accurate term.”
Of people self-reporting gluten or wheat sensitivity, only around 16 per cent show symptoms when subjected to a clinical trial to replicate the response.
Moving forward, the team emphasised the need for further research to ensure future testing is equipped to differentiate between coeliac disease and NCG/WS.
Read the full MJA article here
Related news
- Former Australian Prime Minister honoured at University of Newcastle graduations
- Breaking barriers: First doctors graduate from equity pathway
- Advancing Human-Agent Collaboration Through Agentic AI
- Translating compassion: a linguist's commitment to social inclusion
- From Research to Reality: New Algorithms Revolutionise Geotechnical Design
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.