Improving outcomes for regional stroke patients
Clinical researchers at the University of Newcastle have found ways to overcome traditional treatment barriers experienced by stroke patients in regional and rural communities.
Researchers from the University of Newcastle have collaborated with clinicians in the NSW Hunter Valley on two major interventions that are benefiting stroke patients who live outside our major cities.
In 2007, renowned stroke experts Professor Mark Parson and Professor Chris Levi partnered with Hunter New England Local Health District to develop Australia’s first Pre-hospital Acute Stroke Triage (PAST) protocol for metropolitan areas. The team trialled adapted protocols for regional and rural areas in 2012. They also pioneered the use of advanced multimodal CT brain imaging.
These interventions delivered:
- improved access to thrombolysis for targeted patients
- improved patient selection for acute stroke treatment
- clinical and economic benefits for the NSW Health system.
The team’s research has also shaped national and state-based stroke management policy.
The problem
Stroke is the second leading cause of death worldwide and the leading cause of long-term adult disability in Australia.
Intravenous alteplase has a treatment window of 4.5 hours from the onset of stroke. However, there are barriers to effective implementation, including processes to support the rapid transit of stroke patients to local hospitals and then to the point of therapy within the facility.
Residents in rural areas face the greatest barriers to treatment. Small hospitals are further challenged by the need for a stroke expert to review patients and decide on subsequent administration of thrombolysis, yet these experts rarely exist in small communities. Professor Parson's and Levi led the charge to make positive change.
PAST protocol for regional areas
The rural PAST protocol trial of 2012 involved patients and hospitals in NSW’s Upper Hunter, Great Lakes and Manning regions – areas that did not previously have access to pre-hospital stroke thrombolysis.
Researchers tested a package of interventions, including a customised pre-hospital stroke assessment tool, stroke team pre-notification, hospital bypass orders and rapid stroke team deployment. The trial used both road and a mix of road and helicopter patient transports.
During the study, 470 strokes occurred in the catchment area, with 40 patients transported under the rural protocol to John Hunter Hospital in Newcastle. Fifteen of these patients received thrombolysis, which represented a 3.2% increase in thrombolytic access for rural patients.
An economic evaluation of the rural protocol was conducted with support from the university’s Centre for Clinical Epidemiology and Biostatistics and the Hunter Medical Research Institute. It showed eligible patients were 17 times more likely to receive thrombolysis because of the rural protocol.
The interventions were also associated with an estimated net avoidance of 93.3 disability-adjusted life years (DALYs). The average cost per DALY averted patient in the intervention group compared to the control was around $10,900. That suggests a potential cost savings of $4 million for the Hunter region over a 12-month period.
The rural PAST protocol has since been incorporated into the NSW Agency for Clinical Innovation’s Statewide Reperfusion Program in 2013.
Advanced imaging support to help stroke patients in small hospitals
Smaller regional and rural hospitals often lack on-site stroke experts, which are needed to adequately diagnose and treat acute patients.
To overcome this shortfall in the Hunter region, Professor Parson's and Levi, their colleagues and clinicians at Hunter New England Health worked together to link the 24/7 tele-health service available at John Hunter Hospital to smaller hospitals in Manning and Taree.
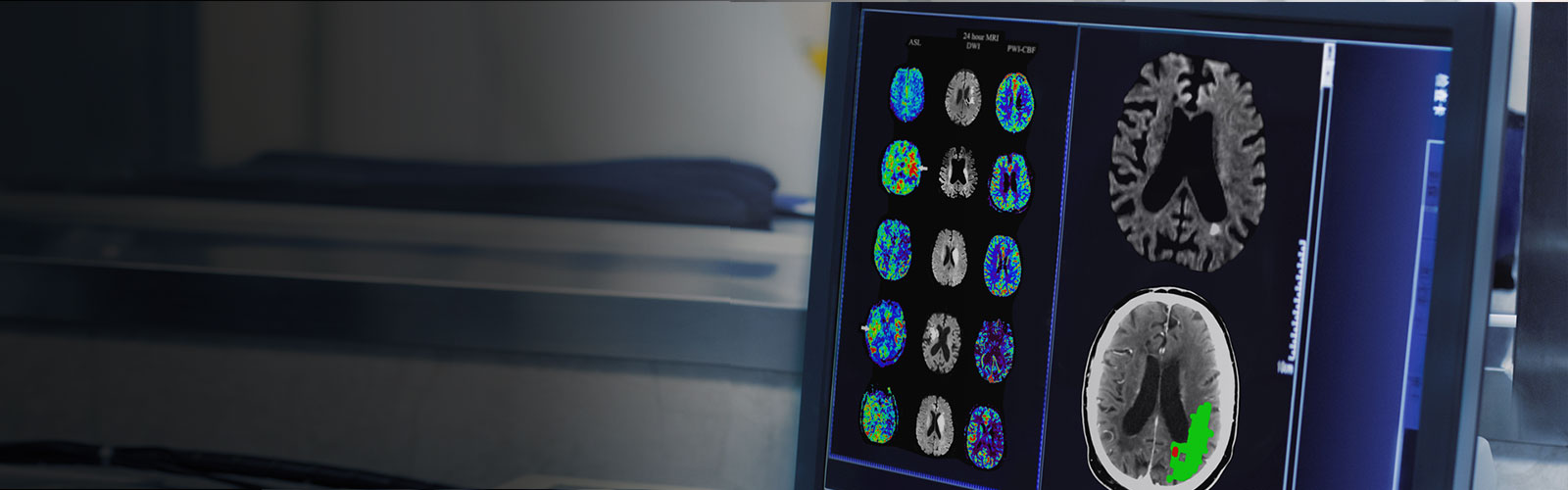
Recent advances in stroke therapies require advanced imaging to rapidly identify eligible patients for appropriate treatment. Conventional telehealth services only use non-contrast CT imaging to exclude the presence of a haemorrhage before treatment decision. In this trial, researchers used more advanced multimodal CT imaging.
During the trial period, clinicians used traditional tele-stroke with 58 patients. They identified 41 as acute stroke and 17 as mimics. The advanced imaging identified a further eight patients who were originally determined to be unsuitable for thrombolysis, thus preventing potentially adverse outcomes for those individuals. In addition, 40 percent of the treated patients were discharged with nil to mild side effects.
The trial showed that the use of advanced imaging was not only as safe and efficient as traditional tele-stroke services – it also improved patient selection for thrombolysis.
This application of advanced multimodal CT brain imaging in regional centres was included in the national acute stroke care guidelines in 2015.
For information:
Conjoint Professor Chris Levi
christopher.levi@newcastle.edu.au
(02) 4921 3490
Professor Neil Spratt
(02) 4921 6171

Conjoint Professor Chris Levi
The team’s research has also shaped national and state-based stroke management policy.
Aligned with the United Nations Sustainable Development Goals
Read more research impact case studies
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.


