Improving survival outcomes for AML using novel approaches
Dr Heather Murray
Acute myeloid leukaemia (AML) is an aggressive and tough-to-cure blood cancer. Through her potentially life-saving work, Dr Heather Murray is developing precision therapies that target the unique biology of AML cells to tackle treatment resistance.
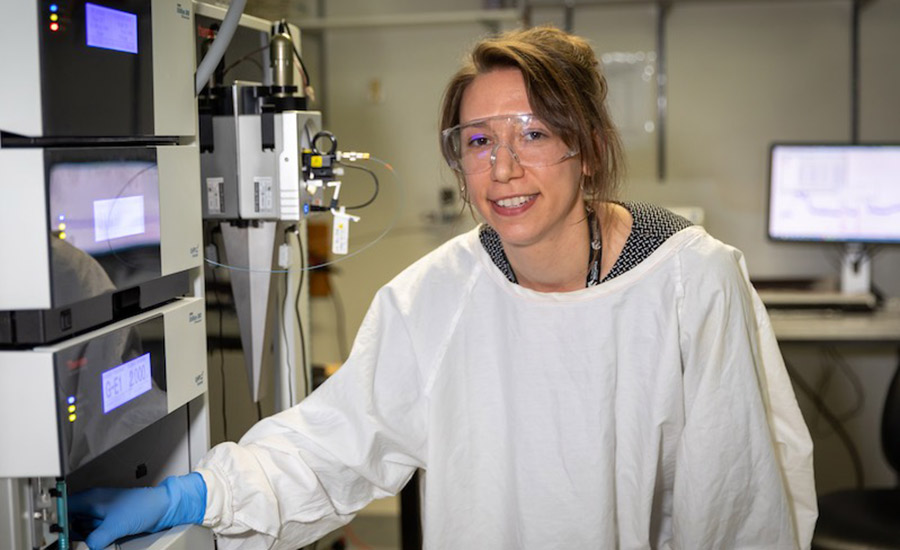
Heather is a postdoctoral cancer researcher at the University of Newcastle, driven by the potential of science to improve treatments for cancer patients.
Originally planning a career in pharmacy, she found her undergraduate degree in biomedical science ignited a passion for research.
“In Biomed, I was exposed to the work of several talented local researchers, and I became interested in the ways that science could be applied to solve biological mysteries and improve treatment outcomes for people who have cancer,” Heather explains.
Her research journey began with summer scholarships and an early focus on melanoma. She later approached Associate Professor Verrills, eager to pursue a PhD project with maximum translational impact.
“I chose to work on leukaemia biology because it was unlike anything I’d done before and had the potential to make a huge difference,” she says.
Heather was awarded her doctorate by the University of Newcastle in 2020. A postdoctoral research position in the team of Associate Professor Verrills followed.
Heather’s PhD study into a novel therapeutic strategy for AML with mutations in the tyrosine kinase 3 (FLT3) gene, which is mutated in approximately one-third of AML cases, has garnered international attention.
Heather is the lead author of research findings from a collaboration between the University of Newcastle, Hunter Medical Research Institute, Hunter Cancer Research Alliance, and the University of Southern Denmark.
In 2021, these findings were published in Leukemia, a prestigious international journal specialising in blood cancer.
Progress in an underexplored area
Each year, approximately 1,100 Australians are diagnosed with acute myeloid leukaemia (AML), a disease that predominantly affects older adults.
AML is one of the most aggressive blood cancers, with a 5-year survival rate of less than 30 per cent. Heather’s research focuses on improving survival outcomes for AML patients by exploring novel approaches to overcome treatment resistance.
“Because AML is relatively rare, it hasn’t received as much research focus as more common cancers,” says Heather.
“The onset of symptoms is very sudden, and the disease progresses rapidly, making treatment selection challenging. However, survival rates have been steadily increasing, and I’m hopeful that further research will continue this trend.”
Targeting a DNA repair protein
“Every individual’s leukaemia is different”, shares Heather. “This reality means that a treatment that works for one person might not be effective for another.”
“Because of this, we need to develop precision therapies tailored to each patient’s cancer. This involves identifying the specific features of AML cells that drive their growth, division and spread.”
“From here, we try and develop tailored therapies targeting these specific features,” she explains.
Analysing cancer cells through methods like proteomics, phosphoproteomics, and genetic mutation studies offers deep insights into cancer biology.
Phosphoproteomics, which examines protein modifications like phosphorylation (a ‘cellular on-off switch’), is particularly useful when combined with other techniques.
In a recent study, the team focused on analysing cells with a KIT gene mutation found in about 5 per cent of acute myeloid leukemia (AML) cases.
Their findings reveal that DNA-dependent protein kinase (DNA-PK) remains continuously active in leukemia cells with the KIT mutation. As a result, they explore the effect of inhibiting both mutant KIT and DNA-PK to halt the growth of these cancerous cells.
By combining standard-of-care drugs with a DNA-PK inhibitor, the treatment significantly reduced leukemia cells while sparing healthy ones.
Heather and her team are optimistic that this strategy, which minimises side effects early in the drug development process, will lead to a well-tolerated therapy.
She hopes her findings will quickly translate into clinical trials to accelerate the discovery of new treatments.
Seeking a clinician’s expertise
The team’s work involves working closely with clinician-researcher Associate Professor Anoop Enjeti, who brings unique insight to our work, making sure they’re always working towards the goal of taking their work into the clinic.
The collaboration with Dr Enjeti is also crucial to the process of testing potential therapies by facilitating the collection of patient cell donations.
“If a patient arrives at the clinic and they consent for some of their samples being used for our research, we can then analyse these cells in the lab and test their response to potential new therapies”, Heather explains.
Importance of research funding
Despite her successes in the field so far, Heather shares that being an emerging researcher comes with the challenge of balancing multiple responsibilities.
These include applying for grants to secure research funding, supervising staff and students, managing research projects, and spending time in the lab conducting experiments.
In a competitive field like this, securing funding as a new researcher can be particularly tough. But it’s so important.
In 2022, Heather received a Cancer Institute NSW fellowship to pursue research into new therapeutic targets for AML.
In 2023, Heather and her team secured a grant to investigate drug resistance in AML, generously funded by Cure Cancer's BarbeCURE®. And her funding was extended in 2024, thanks to the people at Bobbin Head Cruising Club.
“Funding like this enables me to keep working toward more effective precision therapies for AML patients. By investing in early-career researchers, you’re not only driving crucial cancer research forward but also helping to shape the future of scientific discovery.”
Driven by each diagnosis
The groundbreaking work of Heather and her team shines a ray of hope for AML patients in their battle against this formidable cancer.
This potential to help those in need of effective treatment solutions for leukaemia drives her research—every day, she feels it’s real, raw purpose.
“Each time a new sample arrives in the lab, I’m reminded that these cancer cells come from a patient—someone’s parent, sibling, or friend. Someone whose life has been turned upside down by this diagnosis. This motivates me to keep working towards a cure.”
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.