Researcher Highlights
Signalling a new future for leukaemia treatment
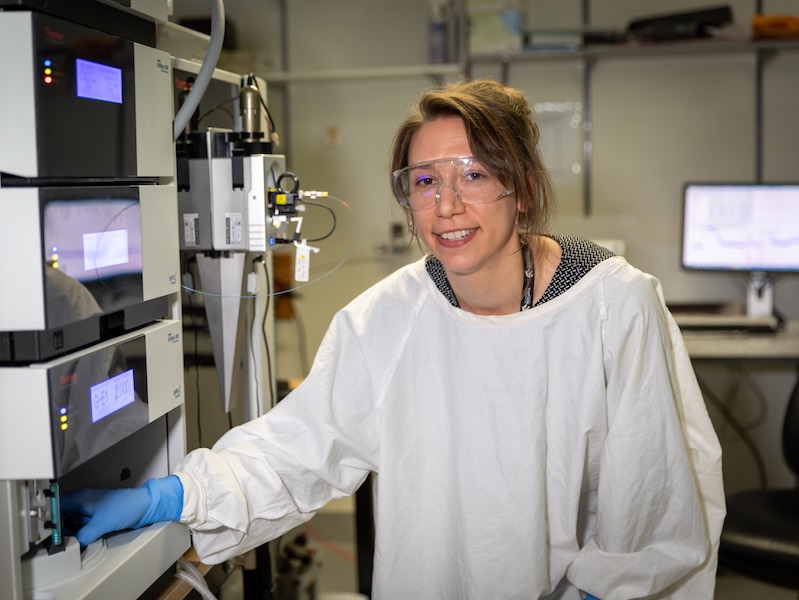
Heather Murray
Despite only recently beginning her research career, Dr Heather Murray has already identified a puzzle piece that could revolutionise the quest for more effective treatment of acute myeloid leukaemia (AML).
Only one in four patients treated for acute myeloid leukaemia (AML), the most aggressive subtype of blood cancer, will survive five years past their diagnosis.
Recent advances in cancer research have improved outcomes, with a focus on genomic-based cell analyses informing customised treatment for each individual patient.
In partnership with key international collaborators, cancer researchers at UON, HMRI and the Hunter Cancer Research Alliance, are taking this research a step further by using proteomics to study proteins, and erroneous signaling, with the hope of identifying potential therapies.
The newest addition to this group of ground breaking collaborators is postdoctoral researcher Dr Heather Murray.
Setting the course
Initially planning a career in pharmacy, Heather found her undergrad degree in biomedical science provided the inspiration to follow a research path.
“In biomed I was exposed to the work of several talented local researchers, and I became interested in the ways that science could be applied to solve biological mysteries and improve treatment outcomes for people suffering with cancer,” Heather explains.
Continuing a study trajectory encompassing undergrad Summer scholarships and an early focus on melanoma, Heather sought out Associate Professor Verrills in a bid to take on a PhD project with maximum translational potential.
“I chose to work on a project researching leukaemia biology because it was different to anything I had done before, and could have massive impact,” Heather says.
Heather was awarded her doctorate by the University of Newcastle in 2020. A postdoctoral research position in the team of Associate Professor Verrills followed.
Heather’s PhD study into a novel therapeutic strategy for AML with mutations in the tyrosine kinase 3 (FLT3) gene, which is mutated in approximately one third of AML cases, has garnered international attention.
A research collaboration between researchers from the University of Newcastle, Hunter Medical Research Institute and Hunter Cancer Research Alliance, and the University of Southern Denmark, Heather is lead author on these findings, recently published in the prestigious international blood cancer journal Leukemia.
Inhibiting AML
In AML, overactive signaling prevents white blood cells from maturing and developing the power to fight infection. Simultaneously, the AML cells divide and grow at accelerated rates, taking over the blood and bone marrow and impeding healthy immune system processes.
Heather hypothesized that identifying unusually active cell proteins could provide invaluable clues to possible targets for therapeutic inhibition.
“I utilised phosphoproteomics to investigate not just whether the protein was there, but I was looking for a phosphorylation state which is a modification on the protein which generally indicates that the protein is active,” Heather says.
“We found that a protein called DNA-PK was highly phosphorylated in mutant FLT3 AML. So that suggested to us that DNA-PK may be highly active in the leukaemia, and therefore targeting DNA-PK would be an effective therapeutic strategy.”
Startling preclinical results suggest that using chemical compounds to simultaneously block the activity of FLT3 and DNA-PK causes the leukaemia cells to die whilst having no effect on normal, healthy cells.
Where to from here
Whilst working toward clinical trials with this new knowledge, Heather and her cancer research collaborators will be looking at whether this combination of inhibitors is relevant in the treatment of other forms of blood cancer, as well as investigating the efficacy of this novel strategy in regard to drug resistance.
“Our working hypothesis is that adding the DNA-PK inhibitor may actually reduce development of resistance,” Heather says.
“We do have funding from the NHMRC to do further work, to look at resistance to the targeted therapies that we’re using and whether we can possibly target pathways to prevent resistance from happening.”
To maximise and streamline experiments using donor cells, the Hunter Leukaemia Program has been established.
“We work closely with clinician researcher Associate Professor Anoop Enjeti, who brings unique insight to our work, making sure we are always working towards taking our work into the clinic,” Heather says.
The collaboration with Dr Enjeti is also crucial to the process of testing potential therapies by facilitating the collection of patient cell donations.
“If a patient arrives to clinic and they consent for some of their sample being used for our research, we can then analyse these cells in the lab and test their response to potential new therapies.”
Heather is dedicated to her research and finds purpose in the possibility of helping those who need effective treatment solutions for leukaemia.
“I find medical research rewarding with the potential to make a difference to peoples’ lives. I am drawn to the problem-solving aspect of research work, whilst the prospect of contributing to improved health and medical treatment in the community also drives my enthusiasm and commitment.”
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.