Australia’s Omicron wave earlier this year was much larger than we thought, recent research has confirmed. We also heard Health Minister Mark Butler acknowledge Australia can expect a “very big wave” of people with long COVID over the next few years.

Doctors and researchers have been warning about the growing threat of long COVID, as restrictions ease and case numbers climb.
So we need to take an urgent look at how we manage and treat it.
Remind me again, what’s long COVID?
More than 7 million Australians have had COVID; most have recovered from the acute illness. But some have lingering symptoms for months, or longer.
The World Health Organization defines long COVID as symptoms present three months after infection, lasting at least two months, that cannot be attributed to other diagnoses.
The most common symptoms include: fatigue, especially after activity, shortness of breath, brain fog or difficulty concentrating, sleep problems, chronic cough, muscle aches and pains, loss of smell or taste, depression and anxiety.
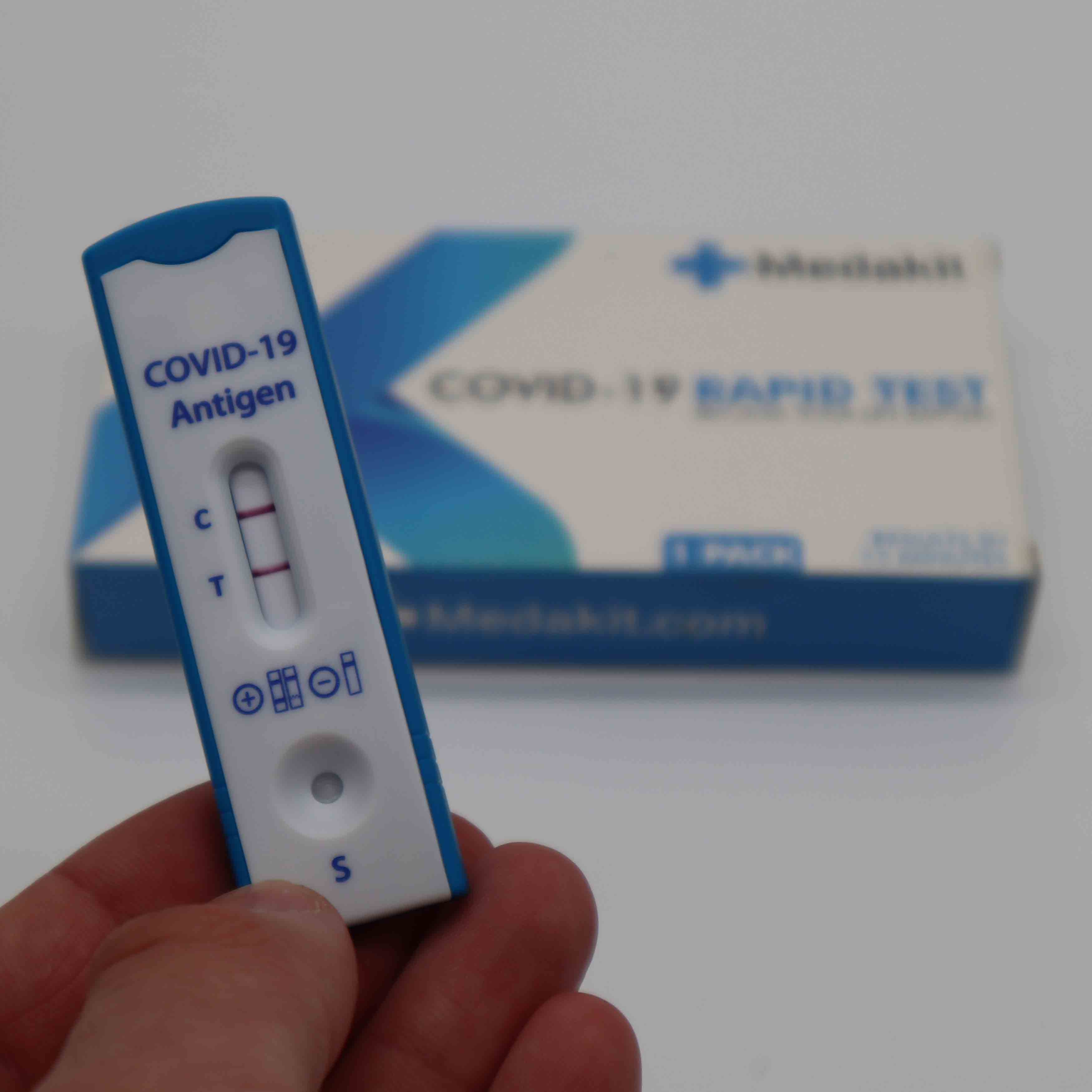
But there is no one test that diagnoses long COVID. So this multitude of complex symptoms makes it a difficult condition to track down, study and treat.
Who’s more likely to get long COVID?
The risk of long COVID is increased in people who have had more severe COVID, women and people with a chronic illness, such as diabetes, or chronic lung or heart disease.
A US study looked at 4.5 million people treated in the community or in hospital, and followed them to see if they developed long COVID. At six months, 7% had symptoms.
Worryingly this study also suggests being vaccinated only reduced the risk of long COVID by 15%. Symptoms such as brain fog and fatigue were present and vaccination seemed only partly protective against them.
How do we treat long COVID?
Australia’s National COVID-19 Clinical Evidence Taskforce’s recommendations for treating long COVID were updated in May. But these borrow heavily from UK recommendations and the evidence backing these recommendations is at best weak.
In the UK “long COVID clinics” have adopted a medical-led holistic model of care. This involves GPs, specialists and allied health workers, such as physiotherapists, occupational therapists and exercise physiologists. Similar clinics have been set up in Australia.
However, the advice for such clinics is based on consensus and experience of similar conditions, such as chronic fatigue, and what we know about how people recover after leaving intensive care, rather than the results of robust studies focusing on long COVID.
UK advice for treating long COVID involves looking for and managing COVID complications that may affect the lungs, lead to heart disease and managing other existing conditions, such as obesity and diabetes. It also recommends assessing and managing anxiety and depression, which not surprisingly is common in people with long COVID.
UK guidelines advise supporting people to manage their own symptoms, including getting support from their GP, then referral to specialist services when needed.
If people had COVID pneumonia – especially those who went to intensive care, still have breathing problems and are weak – there is some limited evidence pulmonary rehabilitation helps. This is out-patient care with specialist physiotherapists and nurses, involving breathing exercises, education and support.
Two small trials have shown pulmonary rehabilitation, improves breathlessness, exercise capacity, fatigue and quality of life. So this is now recommended.
Related Articles

Giving men a common antidepressant could help tackle domestic violence: world-first study
In April 2024, Prime Minister Anthony Albanese declared domestic and family violence a “national crisis” calling for proactive responses that “focus on the perpetrators and focus on prevention”.The issue hasn’t really improved since then.
Read more

What is gingivitis? How do I know if I have it?
Do your gums look red and often bleed when you brush them, but they’re not painful? If so, you could have the gum disease gingivitis.
Read more

Not all processed foods are bad for you. Here’s what you can tell from reading the label
If you follow wellness content on social media or in the news, you’ve probably heard that processed food is not just unhealthy, but can cause serious harm.
Read more

Kids need to floss too, even their baby teeth. But how do you actually get them to do it?
A survey from the Australian Dental Association out this week shows about three in four children never floss their teeth, or have adults do it for them.
Read more

‘Perfect bodies and perfect lives’: how selfie-editing tools are distorting how young people see themselves
Like many of her peers, Abigail (21) takes a lot of selfies, tweaks them with purpose-made apps, and posts them on social media. But, she says, the selfie-editing apps do more than they were designed for.
Read more

Pathway to purpose
From limited beginnings to limitless dreams - equity in education is giving Arthur Demetriou the chance to change the face of medicine.
Read more
How to manage fatigue, pain and brain fog?
However, breathing problems are only one component of long COVID.
For people with long COVID and severe fatigue or pain following exertion, a standard exercise program may make things worse. Here, the recommendation is for an initial period of rest then incremental increase in activity, often over many months. However, the optimal approach is not defined.
Neurological symptoms of poor concentration or brain fog, sleep disturbance and altered taste are common, but as yet there are no agreed or proven therapies.
Some people with the most severe neurological symptoms and fatigue develop a disabling condition known as postural orthostatic tachycardia syndrome or POTS. When people stand up, their heart races and blood pressure falls. This leads to severe fatigue, headaches and difficulty concentrating.
This condition can be treated by modifying someone’s diet and taking medication. We know this because we see POTS after other infectious diseases or other prolonged, severe diseases that lead to hospitalisation. However, we need clinical trials for these therapies for long COVID to see which treatments work and for whom.

What’s in the future
There are many aspects of long COVID that health authorities, doctors and researchers have yet to pin down.
We still don’t know what causes long COVID, we don’t have a universally accepted definition of it, robust data to say how many Australians are or will be affected, nor a concrete plan of how to manage the many thousands of cases we can expect. So evidence-based treatments for long COVID are only part of the picture.
But the problem we face is here now. We cannot wait for gold-standard evidence to come in before we start treating people.
In the meantime, people need reliable information about the symptoms of long COVID, what to expect and where to go for help. And health professionals need to take their symptoms seriously.
Health professionals also need training in how to manage people with long COVID, targeting appropriate investigations and treatments that will benefit people the most.
That does not just mean specialised long COVID clinics in capital cities, though it is likely we will need these to help people with the most debilitating problems.
This article is republished from The Conversation under a Creative Commons license. Read the original article.

