
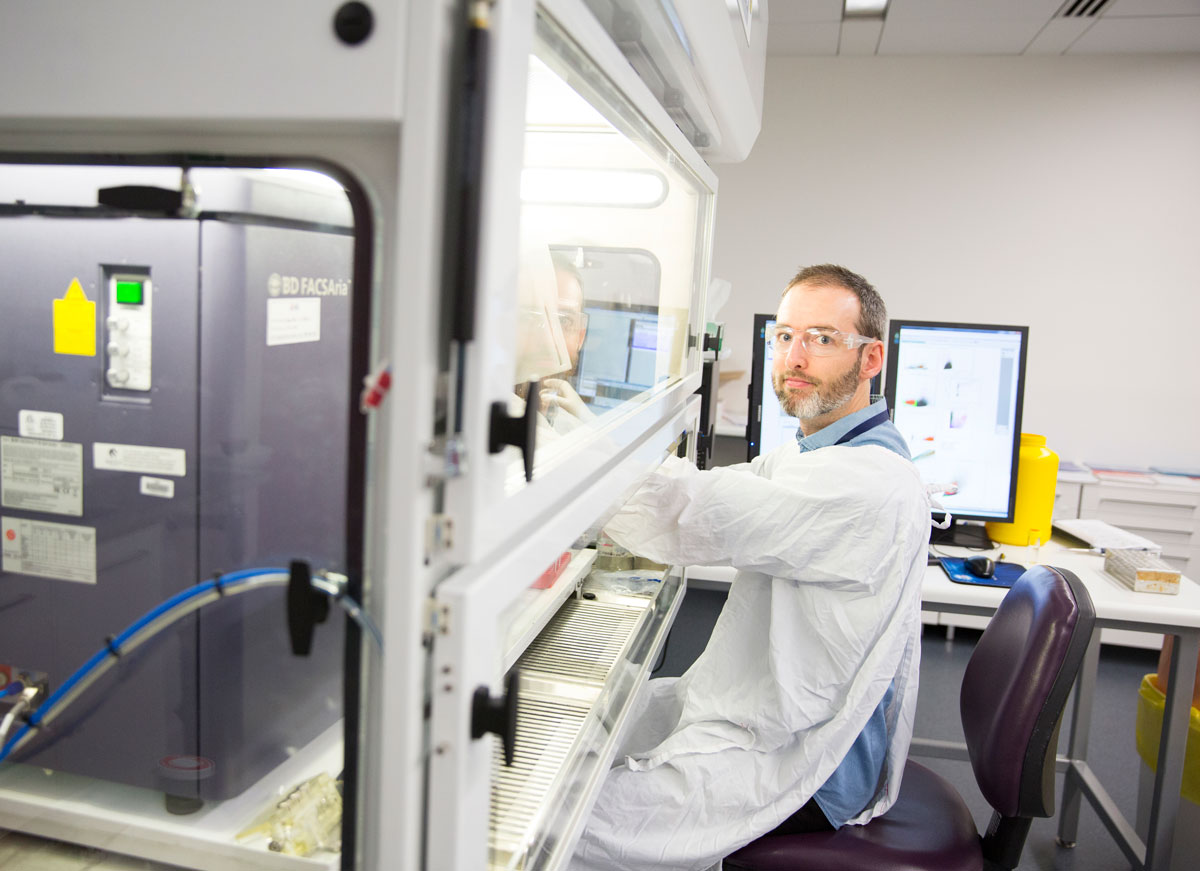
Dr Michael Fricker
Postdoctoral Research Fellow
School of Medicine and Public Health
- Email:michael.fricker@newcastle.edu.au
- Phone:(02) 4042 0207
Understanding the molecular basis of disease
Dr Michael Fricker started his academic career at the University of Cambridge, where he studied cell death in brain cells, first as a PhD student and then as a post-doctoral researcher. He’s now using those cell biology techniques to investigate the causes of asthma and chronic obstructive pulmonary disease (COPD) at the University of Newcastle.
“I would describe myself as a cell biologist – before I moved to the HMRI, most of my work was done in basic sciences, trying to understand the molecular mechanisms by which cells die.”
His research group at Cambridge was the first to identify a novel form of cell death, ‘phagoptosis’.
“A popular idea in cell death research is that cells die and then (and only then) they're eaten by neighbouring cells. We discovered that actually the eating process itself can drive death, so if you block the eating then you can rescue cells in certain situations.”
“This has important implications in medical research. In our bodies, an estimated 70 billion cells die per day. These death pathways are highly regulated as part of the body’s internal homeostasis mechanisms. Disruption of this regulation is manifested in a number of medical conditions – from neurodegeneration to cancer to asthma.”
New challenges
Michael moved to Newcastle in 2012, where he worked alongside Professor Phil Hansbro at UON’s Centre for Asthma & Respiratory Disease (now PRC for Healthy Lungs).
“It was quite a big change of field for me and a big challenge but I learned a lot."
“I have been able to apply some of my expertise in those basic cellular processes to our research on respiratory disease. So we have projects looking at different types of cell death in COPD – lung structures are destroyed and certain types of cell death can contribute to that as well as the ongoing inflammation in the lungs.”
Focus on severe asthma
Since 2016, Michael has been working with Professor Peter Gibson at the university’s Centre of Excellence for Severe Asthma, alongside translational health researchers and lab-based scientists alike.
“We’re working at both ends of the spectrum. I’m looking for biomarkers and we’re also looking at ways to translate this medical research into clinical practice.”
Asthma is an umbrella term which encompasses a number of subtypes of the disease. Severe asthma patients display the most extreme clinical symptoms, which are typically resistant to conventional drug treatments.
“We’re specifically targeting severe asthma because that's the area where there's the most unmet clinical need.”
There are a number of emerging asthma drugs on the market, and a number of them which have shown promise in clinical trials target ‘type 2 inflammation’. While approximately 50% of asthma patients exhibit this type of inflammation and are therefore likely to benefit from these drugs, there is a lot less known about the inflammatory processes observed in the rest of the asthmatic population.
“I'm aiming to understand some of those processes, develop biomarkers that report them and hopefully help to uncover new therapeutic targets. So what we're trying to do is develop ways of better managing the disease and better ways of using these new treatments that are coming through.”
Rethinking sputum subtypes
Currently, asthma subtypes and corresponding treatment pathways are designated using microscopy analysis of patient sputum samples.
“Conventional sputum analysis is performed using a microscope based cell count – so the only information that goes into that process is whatever is distinguishable by eye.”
Michael is currently researching ways to improve this subtyping process, with the ultimate goal of delivering personalised medicine to severe asthma patients.
“While we might count a few hundred cells under a microscope, if we were to run that same sample on a flow cytometer, we might count a couple of million cells. That way, we can look at rarer cells, like mast cells - which are linked to allergic inflammation.”
Flow cytometers can rapidly identify cells based on their size and density. Researchers can also label different cell types by using targeted stains which correspond to specific cell markers.
“It hasn't been used very much in clinical studies; in part because the technology is relatively new and in part because sputum is sticky stuff, which creates a further technical challenge. While it isn't suitable for mass clinical use at the moment, it's an evolving technology and we are generating some very promising results.”
Another application for flow cytometry in this context is the isolation of specific cells from patient samples. These cells can then be closely studied in the lab.
By investigating disease subtypes at the molecular level, Michael is hoping to identify specific biomarkers to guide treatment pathways.
“My overriding passion is the study of basic cellular processes and life at that cellular and molecular level. We can learn a lot about these basic processes through studying disease as well - and the two are fully interconnected.”
Understanding the molecular basis of disease
Michael Fricker is a post-doctoral research fellow within the Centre of Excellence for Severe Asthma.
Career Summary
Biography
I am a senior post-doctoral research fellow working within the Respiratory Medicine research group at HMRI. I lead a research program discovering and validating novel cellular and molecular mechanisms of disease and biomarkers in asthma and chronic obstructive pulmonary disease (COPD). I am currently principal investigator of the ALTEOS trial, a three year prospective clinical cohort study investigating inflammatory mechanisms in severe asthma. I completed my PhD in cellular neuroscience at the University of Cambridge, UK, in 2008 and subsequently held post-doctoral positions at the Beatson Institute for Cancer Research, Glasgow, UK and at the University of Cambridge.
Research ExpertisePathogenesis of Severe Asthma and COPD. Advanced single cell and 'omic analyses of clinically derived airway and blood samples. Macrophages, mast cells and their roles in disease. Molecular analysis of cell death pathways including apoptosis, necrosis, necroptosis, phagoptosis, phagocytosis. Metabolic flux analysis. Mechanisms of neurodegeneration and neuroprotection.
Teaching Expertise
I have extensive experience in leading small group tutorials covering a broad range of basic biochemical and genetic topics and their relation to disease. I have also assisted and led laboratory-based undergraduate practical classes, facilitating results analysis and discussion in large and small teaching groups. I have supervised five PhD, two honours students and one masters student to completion and am currently primary supervisor or co-supervisor of three PhD students.
Qualifications
- PhD, University of Cambridge - UK
Keywords
- Asthma
- Biochemistry
- COPD
- Cachexia
- Cell Biology
- Cell Death
- Efferocytosis
- Human Disease
- Inflammation
- Macrophage
- Mast Cell
- Microglia
- Neurodegeneration
- Pulmonary disease
Fields of Research
| Code | Description | Percentage |
|---|---|---|
| 320103 | Respiratory diseases | 40 |
| 320407 | Innate immunity | 60 |
Professional Experience
Academic appointment
| Dates | Title | Organisation / Department |
|---|---|---|
| 24/3/2018 - 21/10/2021 | TSANZ/AstraZeneca post-doctoral research fellow | University of Newcastle School of Medicine and Public Health Australia |
| 16/5/2016 - | NHMRC Post-doctoral Research Fellow | University of Newcastle School of Medicine and Public Health Australia |
| 14/5/2012 - 14/5/2016 | Post-doctoral research associate | The University of Newcastle School of Biomedical Sciences and Pharmacy Australia |
| 1/1/2009 - 1/4/2012 | Post-doctoral researcher | University of Cambridge Department of Biochemistry United Kingdom |
| 1/1/2008 - 1/1/2009 | Post-doctoral researcher | Beatson Cancer Research Institute Cancer Cell Death laboratory United Kingdom |
Awards
Award
| Year | Award |
|---|---|
| 2018 |
Vice-Chancellor's Award for Collaboration Excellence The University of Newcastle |
| 2018 |
PRC for Healthy Lungs Outstanding Scholar Priority Research Centre (PRC) for Healthy Lungs | The University of Newcastle |
Prize
| Year | Award |
|---|---|
| 2015 |
AstraZeneca Innovation Prize for best basic science presentation - Newcastle Asthma Meeting 2015 Newcastle Asthma Meeting |
Publications
For publications that are currently unpublished or in-press, details are shown in italics.
Chapter (2 outputs)
| Year | Citation | Altmetrics | Link | ||
|---|---|---|---|---|---|
| 2019 |
Baines K, Simpson J, Fricker M, Gibson P, 'Biology of Neutrophils', Middleton's Allergy 2-Volume Set Principles and Practice, Elsevier, USA (2019)
|
||||
| 2011 |
Fricker M, Tolkovsky A, 'Necrosis, Apoptosis, and Autophagy: Mechanisms of Neuronal and Glial Cell Death', Cell Culture Techniques, Neuromethods, Springer, London, UK 305-330 (2011) [B1]
|
Journal article (48 outputs)
| Year | Citation | Altmetrics | Link | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 2024 |
Budden KF, Shukla SD, Bowerman KL, Vaughan A, Gellatly SL, Wood DLA, et al., 'Faecal microbial transfer and complex carbohydrates mediate protection against COPD.', Gut, 73 751-769 (2024) [C1]
|
Nova | |||||||||
| 2024 |
Toennesen B, Schmid JM, Sorensen BS, Fricker M, Hoffmann HJH, 'A five-gene qPCR signature can classify type 2 asthma comparably to microscopy of induced sputum from severe asthma patients', EUROPEAN CLINICAL RESPIRATORY JOURNAL, 11 (2024) [C1]
|
Nova | |||||||||
| 2022 |
Niessen NM, Fricker M, McDonald VM, Gibson PG, 'T2-low: what do we know? Past, present, and future of biologic therapies in noneosinophilic asthma', ANNALS OF ALLERGY ASTHMA & IMMUNOLOGY, 129 150-159 (2022) [C1]
|
Nova | |||||||||
| 2022 |
Liu G, Jarnicki AG, Paudel KR, Lu W, Wadhwa R, Philp AM, et al., 'Adverse roles of mast cell chymase-1 in chronic obstructive pulmonary disease.', European Respiratory Journal, 60 2101431-2101431 (2022) [C1]
|
Nova | |||||||||
| 2022 |
Liu G, Jarnicki AG, Paudel KR, Lu W, Wadhwa R, Philp AM, et al., 'Adverse roles of mast cell chymase-1 in COPD', EUROPEAN RESPIRATORY JOURNAL, 60 (2022) [C1]
|
Nova | |||||||||
| 2022 |
Fricker M, Qin L, Sánchez-Ovando S, Simpson JL, Baines KJ, Riveros C, et al., 'An altered sputum macrophage transcriptome contributes to the neutrophilic asthma endotype.', Allergy, 77 1204-1215 (2022) [C1]
|
Nova | |||||||||
| 2021 |
Winter NA, Gibson PG, McDonald VM, Fricker M, 'Sputum Gene Expression Reveals Dysregulation of Mast Cells and Basophils in Eosinophilic COPD', INTERNATIONAL JOURNAL OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE, 16 2165-2179 (2021) [C1]
|
Nova | |||||||||
| 2021 |
Skerrett-Byrne DA, Bromfield EG, Murray HC, Jamaluddin MFB, Jarnicki AG, Fricker M, et al., 'Time-resolved proteomic profiling of cigarette smoke-induced experimental chronic obstructive pulmonary disease', Respirology, 26 960-973 (2021) [C1] Background and objective: Chronic obstructive pulmonary disease (COPD) is the third leading cause of illness and death worldwide. Current treatments aim to control symptoms with n... [more] Background and objective: Chronic obstructive pulmonary disease (COPD) is the third leading cause of illness and death worldwide. Current treatments aim to control symptoms with none able to reverse disease or stop its progression. We explored the major molecular changes in COPD pathogenesis. Methods: We employed quantitative label-based proteomics to map the changes in the lung tissue proteome of cigarette smoke-induced experimental COPD that is induced over 8 weeks and progresses over 12 weeks. Results: Quantification of 7324 proteins enabled the tracking of changes to the proteome. Alterations in protein expression profiles occurred in the induction phase, with 18 and 16 protein changes at 4- and 6-week time points, compared to age-matched controls, respectively. Strikingly, 269 proteins had altered expression after 8 weeks when the hallmark pathological features of human COPD emerge, but this dropped to 27 changes at 12 weeks with disease progression. Differentially expressed proteins were validated using other mouse and human COPD bronchial biopsy samples. Major changes in RNA biosynthesis (heterogeneous nuclear ribonucleoproteins C1/C2 [HNRNPC] and RNA-binding protein Musashi homologue 2 [MSI2]) and modulators of inflammatory responses (S100A1) were notable. Mitochondrial dysfunction and changes in oxidative stress proteins also occurred. Conclusion: We provide a detailed proteomic profile, identifying proteins associated with the pathogenesis and disease progression of COPD establishing a platform to develop effective new treatment strategies.
|
Nova | |||||||||
| 2021 |
Niessen NM, Gibson PG, Baines KJ, Barker D, Yang IA, Upham JW, et al., 'Sputum TNF markers are increased in neutrophilic and severe asthma and are reduced by azithromycin treatment', ALLERGY, 76 2090-2101 (2021) [C1]
|
Nova | |||||||||
| 2021 |
Winter NA, Gibson PG, Fricker M, Simpson JL, Wark PA, McDonald VM, 'Hemopexin: A novel anti-inflammatory marker for distinguishing COPD from Asthma', Allergy, Asthma and Immunology Research, 13 450-467 (2021) [C1] Purpose: Systemic inflammatory biomarkers can improve diagnosis and assessment of chronic obstructive pulmonary disease (COPD) and asthma. We aimed to validate an airway disease b... [more] Purpose: Systemic inflammatory biomarkers can improve diagnosis and assessment of chronic obstructive pulmonary disease (COPD) and asthma. We aimed to validate an airway disease biomarker panel of 4 systemic inflammatory biomarkers, a2-macroglobulin, ceruloplasmin, haptoglobin and hemopexin, to establish their relationship to airway disease diagnosis and inflammatory phenotypes and to identify an optimized biomarker panel for disease differentiation. Methods: Participants with COPD or asthma were classified by inflammatory phenotypes. Immunoassay methods were used to measure levels of validation biomarkers in the sera of participants with disease and non-respiratory disease controls. Markers were analyzed individually and in combination for disease differentiation and compared to established biomarkers (C-reactive protein, interleukin-6, and white blood cell/blood eosinophil count). Results: The study population comprised of 141 COPD, 127 severe asthma, 54 mild-moderate asthma and 71 control participants. Significant differences in ceruloplasmin, haptoglobin and hemopexin levels between disease groups and between systemic inflammatory phenotypes were observed. However, no differences were found between airway inflammatory phenotypes. Hemopexin was the best performing individual biomarker and could diagnose COPD versus control participants (area under the curve [AUC], 98.3%; 95% confidence interval [CI], 96.7%-99.9%) and differentiate COPD from asthmatic participants (AUC, 97.0%; 95% CI, 95.4%-98.6%), outperforming established biomarkers. A biomarker panel, including hemopexin, haptoglobin and other established biomarkers, could diagnose asthma versus control participants (AUC, 87.5%; 95% CI, 82.8%-92.2%). Conclusions: Hemopexin can be a novel biomarker with superior diagnostic ability in differentiating COPD and asthma. We propose an anti-inflammatory axis between the airways and systemic circulation, in which hemopexin is a protective component in airway disease.
|
Nova | |||||||||
| 2021 |
Niessen NM, Gibson PG, Simpson JL, Scott HA, Baines KJ, Fricker M, 'Airway monocyte modulation relates to tumour necrosis factor dysregulation in neutrophilic asthma', ERJ OPEN RESEARCH, 7 (2021) [C1]
|
Nova | |||||||||
| 2021 |
Niessen NM, Baines KJ, Simpson JL, Scott HA, Qin L, Gibson PG, Fricker M, 'Neutrophilic asthma features increased airway classical monocytes', CLINICAL AND EXPERIMENTAL ALLERGY, 51 305-317 (2021) [C1]
|
Nova | |||||||||
| 2021 |
Lu Z, Van Eeckhoutte HP, Liu G, Nair PM, Jones B, Gillis CM, et al., 'Necroptosis Signaling Promotes Inflammation, Airway Remodeling, and Emphysema in Chronic Obstructive Pulmonary Disease', AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE, 204 667-681 (2021) [C1]
|
Nova | |||||||||
| 2021 |
Winter NA, Qin L, Gibson PG, McDonald VM, Baines KJ, Faulkner J, et al., 'Sputum mast cell/basophil gene expression relates to inflammatory and clinical features of severe asthma', JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY, 148 428-438 (2021) [C1]
|
Nova | |||||||||
| 2021 |
Fricker M, McDonald VM, Winter NA, Baines KJ, Wark PAB, Simpson JL, Gibson PG, 'Molecular markers of type 2 airway inflammation are similar between eosinophilic severe asthma and eosinophilic COPD', ALLERGY, 76 2079-2089 (2021) [C1]
|
Nova | |||||||||
| 2020 |
Fricker M, Qin L, Niessen N, Baines KJ, McDonald VM, Scott HA, et al., 'Relationship of sputum mast cells with clinical and inflammatory characteristics of asthma', CLINICAL AND EXPERIMENTAL ALLERGY, 50 696-707 (2020) [C1]
|
Nova | |||||||||
| 2020 |
Baines KJ, Fricker M, McDonald VM, Simpson JL, Wood LG, Wark PAB, et al., 'Sputum transcriptomics implicates increased p38 signalling activity in severe asthma', Respirology, 25 709-718 (2020) [C1] Background and objective: Severe asthma is responsible for a disproportionate burden of illness and healthcare costs spent on asthma. This study analyses sputum transcriptomics to... [more] Background and objective: Severe asthma is responsible for a disproportionate burden of illness and healthcare costs spent on asthma. This study analyses sputum transcriptomics to investigate the mechanisms and novel treatment targets of severe asthma. Methods: Induced sputum samples were collected in a cross-sectional study from participants with severe asthma (n = 12, defined as per GINA criteria), non-severe uncontrolled (n = 21) and controlled asthma (n = 21) and healthy controls (n = 15). Sputum RNA was extracted and transcriptomic profiles were generated (Illumina HumanRef-8 V2) and analysed (GeneSpring). Sputum protein lysates were analysed for p38 activation in a validation study (n = 24 asthma, n = 8 healthy) by western blotting. Results: There were 2166 genes differentially expressed between the four groups. In severe asthma, the expression of 1875, 1308 and 563 genes was altered compared to healthy controls, controlled and uncontrolled asthma, respectively. Of the 1875 genes significantly different to healthy controls, 123 were >2-fold change from which four networks were identified. Thirty genes (>2-fold change) were significantly different in severe asthma compared to both controlled asthma and healthy controls. There was enrichment of genes in the p38 signalling pathway that were associated with severe asthma. Phosphorylation of p38 was increased in a subset of severe asthma samples, correlating with neutrophilic airway inflammation. Conclusion: Severe asthma is associated with substantial differences in sputum gene expression that underlie unique cellular mechanisms. The p38 signalling pathway may be important in the pathogenesis of severe asthma, and future investigations into p38 inhibition are warranted as a ¿non-Th2¿ therapeutic option.
|
Nova | |||||||||
| 2020 |
Baines KJ, Negewo NA, Gibson PG, Fu JJ, Simpson JL, Wark PAB, et al., 'A Sputum 6 Gene Expression Signature Predicts Inflammatory Phenotypes and Future Exacerbations of COPD', International Journal of COPD, 15 1577-1590 (2020) [C1] Background: The 6 gene expression signature (6GS) predicts in¿ammatory phenotype, exacerbation risk, and corticosteroid responsiveness in asthma. In COPD, patterns of airway in¿am... [more] Background: The 6 gene expression signature (6GS) predicts in¿ammatory phenotype, exacerbation risk, and corticosteroid responsiveness in asthma. In COPD, patterns of airway in¿ammation are similar, suggesting the 6GS may be useful. This study determines the diagnostic and prognostic ability of 6GS in predicting in¿ammatory phenotypes and exacerbation risk in COPD. Methods: We performed 2 studies: a cross-sectional phenotype prediction study in stable COPD (total N=132; n=34 eosinophilic (E)-COPD, n=42 neutrophilic (N)-COPD, n=39 paucigranulocytic (PG)-COPD, n=17 mixed-granulocytic (MG)-COPD) that assessed 6GS ability to discriminate phenotypes (eosinophilia=3%; neutrophilia=61%); and a prospective cohort study (total n=54, n=8 E-COPD; n=18 N-COPD; n=20 PG-COPD; n=8 MG-COPD, n=21 exacerbation prone (=2/year)) that investigated phenotype and exacerbation prediction utility. 6GS was measured by qPCR and evaluated using multiple logistic regression and area under the curve (AUC). Short-term reproducibility (intra-class correlation) and phenotyping method agreement (¿ statistic) were assessed. Results: In the phenotype prediction study, 6GS could accurately identify and discriminate patients with E-COPD from N-COPD (AUC=96.4%; p<0.0001), PG-COPD (AUC=88.2%; p<0.0001) or MG-COPD (AUC=86.2%; p=0.0001), as well as N-COPD from PG-COPD (AUC=83.6%; p<0.0001) or MG-COPD (AUC=87.4%; p<0.0001) and was reproducible. In the prospective cohort study, 6GS had substantial agreement for neutrophilic in¿ammation (82%, ¿=0.63,p<0.001)and moderate agreement foreosinophilici n¿ammation(78%, ¿=0.42,p<0.001). 6GS could signi¿cantly discriminate exacerbationprone patients (AUC=77.2%; p=0.034). Higher IL1B levels were associated with poorer lung function and increased COPD severity. Conclusion: 6GS can signi¿cantly and reproducibly discriminate COPD in¿ammatory phenotypes and predict exacerbation prone patients and may become a useful molecular diagnostic tool assisting COPD management..
|
Nova | |||||||||
| 2019 |
Fricker M, Gibson PG, Powell H, Simpson JL, Yang IA, Upham JW, et al., 'A sputum 6-gene signature predicts future exacerbations of poorly controlled asthma', Journal of Allergy and Clinical Immunology, 144 51-60.e11 (2019) [C1] Background: Improved diagnostic tools for predicting future exacerbation frequency in asthmatic patients are required. A sputum gene expression signature of 6 biomarkers (6-gene s... [more] Background: Improved diagnostic tools for predicting future exacerbation frequency in asthmatic patients are required. A sputum gene expression signature of 6 biomarkers (6-gene signature [6GS], including Charcot-Leyden crystal galectin [CLC]; carboxypeptidase 3 [CPA3]; deoxyribonuclease 1-like 3 [DNASE1L3]; alkaline phosphatase, liver/bone/kidney [ALPL]; CXCR2; and IL1B) predicts inflammatory and treatment response phenotypes in patients with stable asthma. Recently, we demonstrated that azithromycin (AZM) add-on treatment in patients with uncontrolled moderate-to-severe asthma significantly reduced asthma exacerbations (AMAZES clinical trial). Objectives: We sought to test whether the 6GS predicts future exacerbation and inflammatory phenotypes in a subpopulation of AMAZES and to test the effect of AZM therapy on 6GS expression and prognostic capacity. Methods: One hundred forty-two patients (73 placebo-treated and 69 AZM-treated patients) had sputum stored for quantitative PCR of 6GS markers at baseline and after 48 weeks of treatment. Logistic regression and receiver operating characteristic and area under the curve (AUC) determination were performed on baseline measures, and in an exploratory analysis the predictive value of the 6GS was compared with conventional biomarkers for exacerbation and inflammatory phenotypes. Results: The 6GS significantly predicted all future exacerbation phenotypes tested. Calculated AUCs for the 6GS were significantly greater than AUCs for peripheral blood eosinophil counts, sputum neutrophil counts, and combined sputum eosinophil and neutrophil counts. 6GS AUCs were also numerically but not significantly greater than those for fractional exhaled nitric oxide values and sputum eosinophil counts. AZM treatment altered neither 6GS expression nor the predictive capacity of the 6GS for future exacerbation phenotypes. The 6GS was a significant predictor of airway inflammatory phenotype in this population. Conclusion: We demonstrate that a sputum gene signature can predict future exacerbation phenotypes of asthma, with the greatest biomarker performance in identifying those who would experience frequent severe exacerbations. AZM therapy did not modify 6GS expression or biomarker performance, suggesting the therapeutic action of AZM is independent of 6GS-related inflammatory pathways.
|
Nova | |||||||||
| 2019 |
Erriah M, Pabreja K, Fricker M, Baines KJ, Donnelly LE, Bylund J, et al., 'Galectin-3 enhances monocyte-derived macrophage efferocytosis of apoptotic granulocytes in asthma', RESPIRATORY RESEARCH, 20 (2019) [C1]
|
Nova | |||||||||
| 2019 |
Qin L, Gibson PG, Simpson JL, Baines KJ, McDonald VM, Wood LG, et al., 'Dysregulation of sputum columnar epithelial cells and products in distinct asthma phenotypes', Clinical and Experimental Allergy, 49 1418-1428 (2019) [C1] Background: Dysfunction of the bronchial epithelium plays an important role in asthma; however, its measurement is challenging. Columnar epithelial cells are often quantified, yet... [more] Background: Dysfunction of the bronchial epithelium plays an important role in asthma; however, its measurement is challenging. Columnar epithelial cells are often quantified, yet rarely analysed, in induced sputum studies. Objective: We aimed to test whether sputum columnar epithelial cell proportion and count are altered in asthma, and whether they are associated with clinical and inflammatory variables. We aimed to test whether sputum-based measures could provide a relatively non-invasive means through which to monitor airway epithelial activation status. Methods: We examined the relationship of sputum columnar epithelial cells with clinical and inflammatory variables of asthma in a large retrospective cross-sectional cohort (901 participants with asthma and 138 healthy controls). In further studies, we used flow cytometry, microarray, qPCR and ELISA to characterize sputum columnar epithelial cells and their products. Results: Multivariate analysis and generation of 90th centile cut-offs (=11% or =18.1¿×¿104/mL) to identify columnar epithelial cell ¿high¿ asthma revealed a significant relationship between elevated sputum columnar cells and male gender, severe asthma and non-neutrophilic airway inflammation. Flow cytometry showed viable columnar epithelial cells were present in all sputum samples tested. An epithelial gene signature (SCGB3A1, LDLRAD1, FOXJ1, DNALI1, CFAP157, CFAP53) was detected in columnar epithelial cell-high sputum. CLCA1 mRNA and periostin protein, previously identified biomarkers of IL-13-mediated epithelial activation, were elevated in columnar epithelial cell-high sputum samples, but only when accompanied by eosinophilia. Conclusions & clinical relevance: Sputum columnar epithelial cells are related to important clinical and inflammatory variables in asthma. Measurement of epithelial biomarkers in sputum samples could allow non-invasive assessment of altered bronchial epithelium status in asthma.
|
Nova | |||||||||
| 2019 |
Lokwani R, Wark PAB, Baines KJ, Fricker M, Barker D, Simpson JL, 'Blood neutrophils in copd but not asthma exhibit a primed phenotype with downregulated cd62l expression', International Journal of COPD, 14 2517-2525 (2019) [C1] Purpose: To characterize neutrophils in obstructive airway disease by measuring their surface adhesion molecules and oxidative burst along with characterizing them into different ... [more] Purpose: To characterize neutrophils in obstructive airway disease by measuring their surface adhesion molecules and oxidative burst along with characterizing them into different subsets as per their adhesion molecule expression. Patients and methods: Peripheral blood from adults with COPD (n=17), asthma (n=20), and healthy participants (n=19) was examined for expression of CD16, CD62L, CD11b, CD11c, and CD54, and analyzed by flow cytometry. For oxidative burst and CD62L shedding analysis, CD16 and CD62L stained leukocytes were loaded with Dihydrorhodamine-123 (DHR-123) and stimulated with N-Formylmethionine-leucyl-phenylalanine (fMLF). Neutrophil subsets were characterized based on CD16 and CD62L expression. Marker surface expression was recorded on CD16+ neutrophils as median fluorescence intensity (MFI). Results: Neutrophil surface expression of CD62L was significantly reduced in COPD (median (IQR) MFI: 1156 (904, 1365)) compared with asthma (1865 (1157, 2408)) and healthy controls (2079 (1054, 2960)); p=0.028. COPD neutrophils also demonstrated a significant reduction in CD62L expression with and without fMLF stimulation. Asthma participants had a significantly increased proportion and number of CD62Lbright/CD16dim neutrophils (median: 5.4% and 0.14 × 109/L, respectively), in comparison with healthy (3.54% and 0.12 × 109/L, respectively); p<0.017. Conclusion: Reduced CD62L expression suggests blood neutrophils have undergone priming in COPD but not in asthma, which may be the result of systemic inflammation. The increased shedding of CD62L receptor by COPD blood neutrophils suggests a high sensitivity for activation.
|
Nova | |||||||||
| 2019 |
Liu G, Cooley MA, Jarnicki AG, Borghuis T, Nair PM, Tjin G, et al., 'Fibulin-1c regulates transforming growth factor-beta activation in pulmonary tissue fibrosis', JCI INSIGHT, 4 (2019) [C1]
|
Nova | |||||||||
| 2019 |
Liu G, Mateer SW, Hsu A, Goggins BJ, Tay H, Mathe A, et al., 'Platelet activating factor receptor regulates colitis-induced pulmonary inflammation through the NLRP3 inflammasome', Mucosal Immunology, 12 862-873 (2019) [C1] Extra-intestinal manifestations (EIM) are common in inflammatory bowel disease (IBD). One such EIM is sub-clinical pulmonary inflammation, which occurs in up to 50% of IBD patient... [more] Extra-intestinal manifestations (EIM) are common in inflammatory bowel disease (IBD). One such EIM is sub-clinical pulmonary inflammation, which occurs in up to 50% of IBD patients. In animal models of colitis, pulmonary inflammation is driven by neutrophilic infiltrations, primarily in response to the systemic bacteraemia and increased bacterial load in the lungs. Platelet activating factor receptor (PAFR) plays a critical role in regulating pulmonary responses to infection in conditions, such as chronic obstructive pulmonary disease and asthma. We investigated the role of PAFR in pulmonary EIMs of IBD, using dextran sulfate sodium (DSS) and anti-CD40 murine models of colitis. Both models induced neutrophilic inflammation, with increased TNF and IL-1ß levels, bacterial load and PAFR protein expression in mouse lungs. Antagonism of PAFR decreased lung neutrophilia, TNF, and IL-1ß in an NLRP3 inflammasome-dependent manner. Lipopolysaccharide from phosphorylcholine (ChoP)-positive bacteria induced NLRP3 and caspase-1 proteins in human alveolar epithelial cells, however antagonism of PAFR prevented NLRP3 activation by ChoP. Amoxicillin reduced bacterial populations in the lungs and reduced NLRP3 inflammasome protein levels, but did not reduce PAFR. These data suggest a role for PAFR in microbial pattern recognition and NLRP3 inflammasome signaling in the lung.
|
Nova | |||||||||
| 2018 |
Mateer SW, Mathe A, Bruce J, Liu G, Maltby S, Fricker M, et al., 'IL-6 Drives Neutrophil-Mediated Pulmonary Inflammation Associated with Bacteremia in Murine Models of Colitis', American Journal of Pathology, 188 1625-1639 (2018) [C1] Inflammatory bowel disease (IBD) is associated with several immune-mediated extraintestinal manifestations. More than half of all IBD patients have some form of respiratory pathol... [more] Inflammatory bowel disease (IBD) is associated with several immune-mediated extraintestinal manifestations. More than half of all IBD patients have some form of respiratory pathology, most commonly neutrophil-mediated diseases, such as bronchiectasis and chronic bronchitis. Using murine models of colitis, we aimed to identify the immune mechanisms driving pulmonary manifestations of IBD. We found increased neutrophil numbers in lung tissue associated with the pulmonary vasculature in both trinitrobenzenesulfonic acid¿ and dextran sulfate sodium¿induced models of colitis. Analysis of systemic inflammation identified that neutrophilia was associated with bacteremia and pyrexia in animal models of colitis. We further identified IL-6 as a systemic mediator of neutrophil recruitment from the bone marrow of dextran sulfate sodium animals. Functional inhibition of IL-6 led to reduced systemic and pulmonary neutrophilia, but it did not attenuate established colitis pathology. These data suggest that systemic bacteremia and pyrexia drive IL-6 secretion, which is a critical driver for pulmonary manifestation of IBD. Targeting IL-6 may reduce neutrophil-associated extraintestinal manifestations in IBD patients.
|
Nova | |||||||||
| 2018 |
Fricker M, Goggins BJ, Mateer S, Jones B, Kim RY, Gellatly SL, et al., 'Chronic cigarette smoke exposure induces systemic hypoxia that drives intestinal dysfunction.', JCI insight, 3 1-19 (2018) [C1]
|
Nova | |||||||||
| 2018 |
Haw TJ, Starkey MR, Pavlidis S, Fricker M, Arthurs AL, Nair PM, et al., 'Toll-like receptor 2 and 4 have opposing roles in the pathogenesis of cigarette smoke-induced chronic obstructive pulmonary disease.', American journal of physiology. Lung cellular and molecular physiology, 314 L298-L317 (2018) [C1]
|
Nova | |||||||||
| 2018 |
Fricker M, Tolkovsky AM, Borutaite V, Coleman M, Brown GC, 'Neuronal Cell Death.', Physiological reviews, 98 813-880 (2018) [C1]
|
Nova | |||||||||
| 2017 |
Fricker M, Gibson PG, 'Macrophage dysfunction in the pathogenesis and treatment of asthma', EUROPEAN RESPIRATORY JOURNAL, 50 (2017) [C1]
|
Nova | |||||||||
| 2017 |
Fricker M, Heaney LG, Upham JW, 'Can biomarkers help us hit targets in difficult-to-treat asthma?', Respirology, 22 430-442 (2017) [C1] Biomarkers may be a key foundation for the precision medicine of the future. In this article, we review current knowledge regarding biomarkers in difficult-to-treat asthma and the... [more] Biomarkers may be a key foundation for the precision medicine of the future. In this article, we review current knowledge regarding biomarkers in difficult-to-treat asthma and their ability to guide the use of both conventional asthma therapies and novel (targeted) therapies. Biomarkers (as measured by tests including prednisolone and cortisol assays and the fractional exhaled nitric oxide (NO) suppression test) show promise in the assessment and management of non-adherence to inhaled and oral corticosteroids. Multiple markers of type 2 inflammation have been developed, including eosinophils in sputum and blood, exhaled NO, serum IgE and periostin. Although these show potential in guiding the selection of novel interventions for refractory type 2 inflammation in asthma, and in determining if the desired response is being achieved, it is becoming clear that different biomarkers reflect distinct components of the complex type 2 inflammatory pathways. Less progress has been made in identifying biomarkers for use in difficult-to-treat asthma that is not associated with type 2 inflammation. The future is likely to see further biomarker discovery, direct measurements of individual cytokines rather than surrogates of their activity and the increasing use of biomarkers in combination. If the promise of biomarkers is to be fulfilled, they will need to provide useful information that aids clinical decision-making, rather than being ¿just another test¿ for clinicians to order.
|
Nova | |||||||||
| 2016 |
Neniskyte U, Fricker M, Brown GC, 'Amyloid ß induces microglia to phagocytose neurons via activation of protein kinase Cs and NADPH oxidase', International Journal of Biochemistry and Cell Biology, 81 346-355 (2016) [C1] Alzheimer's disease is characterized by brain plaques of amyloid beta and by neuronal loss, but it is unclear how amyloid beta causes neuronal loss and how to prevent this lo... [more] Alzheimer's disease is characterized by brain plaques of amyloid beta and by neuronal loss, but it is unclear how amyloid beta causes neuronal loss and how to prevent this loss. We have previously shown that amyloid beta causes neuronal loss by inducing microglia to phagocytose neurons, and here we investigated whether protein kinase Cs and NADPH oxidase were involved in this. The loss of neurons induced by amyloid beta in co-cultures of primary glia and neurons was completely prevented by inhibiting protein kinase Cs with Gö6976 or Gö6983. Directly activating protein kinase Cs with phorbol myristate acetate stimulated microglial phagocytosis, and induced neuronal loss mediated by MFG-E8/vitronectin receptor pathway of microglial phagocytosis. Blocking phagocytosis by MFG-E8 knockout or receptor inhibition left live neurons, indicating microglial phagocytosis was the cause of neuronal death. Phorbol myristate acetate stimulated the microglial NADPH oxidase, and inhibiting the oxidase prevented neuronal loss. A physiological activator of NADPH oxidase, fMLP, also induced neuronal loss dependent on microglia. Amyloid beta-induced neuronal loss was blocked by NADPH oxidase inhibitors, superoxide dismutase or Toll-like receptor function-blocking antibodies. The results indicate that amyloid beta induces microglial phagocytosis of neurons via activating protein kinase Cs and NADPH oxidase, and that activating the kinases or oxidase is sufficient to induce neuronal loss by microglial phagocytosis. Thus inhibiting protein kinase Cs or NADPH oxidase might be beneficial in Alzheimer's disease or other brain pathologies involving inflammatory neuronal loss mediated by microglia.
|
Nova | |||||||||
| 2016 |
Gang L, Hsu A, Cooley MA, Jarnicki AG, Nair PM, Haw TJ, et al., 'Fibulin-1 regulates the pathogenesis of tissue remodeling in respiratory diseases', Journal of Clinical Investigation Insight, 1 (2016) [C1]
|
Nova | |||||||||
| 2015 |
Brown GC, Vilalta A, Fricker M, 'Phagoptosis - Cell Death By Phagocytosis - Plays Central Roles in Physiology, Host Defense and Pathology.', Current molecular medicine, 15 842-851 (2015) [C1]
|
Nova | |||||||||
| 2015 |
Baxter PS, Bell KFS, Hasel P, Kaindl AM, Fricker M, Thomson D, et al., 'Synaptic NMDA receptor activity is coupled to the transcriptional control of the glutathione system', Nature Communications, 6 (2015) [C1]
|
Nova | |||||||||
| 2014 |
Hansbro PM, Hamilton MJ, Fricker M, Gellatly SL, Jarnicki AG, Zheng D, et al., 'Importance of mast cell Prss31/transmembrane tryptase/tryptase- in lung function and experimental chronic obstructive pulmonary disease and colitis', Journal of Biological Chemistry, 289 18214-18227 (2014) [C1] Protease serine member S31 (Prss31)/transmembrane tryptase/tryptase-¿ is a mast cell (MC)-restricted protease of unknown function that is retained on the outer leaflet of the plas... [more] Protease serine member S31 (Prss31)/transmembrane tryptase/tryptase-¿ is a mast cell (MC)-restricted protease of unknown function that is retained on the outer leaflet of the plasma membrane when MCs are activated. We determined the nucleotide sequences of the Prss31 gene in different mouse strains and then used a Cre/loxP homologous recombination approach to create a novel Prss31 -/- C57BL/6 mouse line. The resulting animals exhibited no obvious developmental abnormality, contained normal numbers of granulated MCs in their tissues, and did not compensate for their loss of the membrane tryptase by increasing their expression of other granule proteases. When Prss31-null MCs were activated with a calcium ionophore or by their high affinity IgE receptors, they degranulated in a pattern similar to that of WT MCs. Prss31-null mice had increased baseline airway reactivity to methacholine but markedly reduced experimental chronic obstructive pulmonary disease and colitis, thereby indicating both beneficial and adverse functional roles for the tryptase. In a cigarette smokeinduced model of chronic obstructive pulmonary disease, WT mice had more pulmonary macrophages, higher histopathology scores, and more fibrosis in their small airways than similarly treated Prss31-null mice. In a dextran sodium sulfate-induced acute colitis model, WT mice lost more weight, had higher histopathology scores, and contained more Cxcl-2 and IL-6 mRNA in their colons than similarly treated Prss31-null mice. The accumulated data raise the possibility that inhibitors of this membrane tryptase may provide additional therapeutic benefit in the treatment of humans with these MC-dependent inflammatory diseases. © 2014 by The American Society for Biochemistry and Molecular Biology, Inc.
|
Nova | |||||||||
| 2014 |
Fricker M, Deane A, Hansbro PM, 'Animal models of chronic obstructive pulmonary disease', Expert Opinion on Drug Discovery, 9 629-645 (2014) [C1] Introduction: Chronic obstructive pulmonary disease (COPD) is a leading global cause of mortality and chronic morbidity. Inhalation of cigarette smoke is the principal risk factor... [more] Introduction: Chronic obstructive pulmonary disease (COPD) is a leading global cause of mortality and chronic morbidity. Inhalation of cigarette smoke is the principal risk factor for development of this disease. COPD is a progressive disease that is typically characterised by chronic pulmonary inflammation, mucus hypersecretion, airway remodelling and emphysema that collectively reduce lung function. There are currently no therapies that effectively halt or reverse disease progression. It is hoped that the development of animal models that develop the hallmark features of COPD, in a short time frame, will aid in the identifying and testing of new therapeutic approaches. Areas covered: The authors review the recent developments in mouse models of chronic cigarette smoke-induced COPD as well as the principal findings. Furthermore, the authors discuss the use of mouse models to understand the pathogenesis and the contribution of infectious exacerbations. They also discuss the investigations of the systemic co-morbidities of COPD (pulmonary hypertension, cachexia and osteoporosis). Expert opinion: Recent advances in the field mark a point where animal models recapitulate the pathologies of COPD patients in a short time frame. They also reveal novel insights into the pathogenesis and potential treatment of this debilitating disease. © 2014 Informa UK, Ltd.
|
Nova | |||||||||
| 2013 |
Fricker M, Vilalta A, Tolkovsky AM, Brown GC, 'Caspase Inhibitors Protect Neurons by Enabling Selective Necroptosis of Inflamed Microglia', JOURNAL OF BIOLOGICAL CHEMISTRY, 288 9145-9152 (2013) [C1]
|
||||||||||
| 2013 |
Neher JJ, Emmrich JV, Fricker M, Mander PK, Théry C, Brown GC, 'Phagocytosis executes delayed neuronal death after focal brain ischemia', Proceedings of the National Academy of Sciences, 110 (2013) [C1]
|
Nova | |||||||||
| Show 45 more journal articles | |||||||||||
Conference (32 outputs)
| Year | Citation | Altmetrics | Link | ||
|---|---|---|---|---|---|
| 2021 |
Fricker M, Qin L, Sanchez-Ovando S, Simpson J, Baines K, Riveros C, et al., 'SPUTUM MACROPHAGES ARE TRANSCRIPTOMICALLY ALTERED IN NEUTROPHILIC ASTHMA', RESPIROLOGY (2021)
|
||||
| 2021 |
Winter N, Qin L, Gibson P, Mcdonald V, Baines K, Faulkner J, et al., 'VALIDATED SPUTUM MAST CELL/BASOPHIL GENE EXPRESSION MEASURES IN SEVERE ASTHMA', RESPIROLOGY (2021)
|
||||
| 2021 |
Gupta S, Fricker M, Xi Y, Upham J, Simpson J, Grainge C, 'FC GAMMA RECEPTOR (FC gamma R) I EXPRESSION IS INCREASED IN SEVERE ASTHMA PARTICULARLY IN PARTICIPANTS WITH NON-EOSINOPHILIC AIRWAY INFLAMMATION', RESPIROLOGY (2021)
|
||||
| 2015 |
Hardingham GE, Baxter P, Bell K, Hasel P, Kaindl A, Thomson D, et al., 'SYNAPTIC NMDA RECEPTOR ACTIVITY IS COUPLED TO THE TRANSCRIPTIONAL CONTROL OF THE GLUTATHIONE SYSTEM IN THE DEVELOPING FOREBRAIN', SCHIZOPHRENIA BULLETIN (2015) [E3]
|
||||
| 2015 | Emmrich J, Vilalta A, Fricker M, Neher J, Brown G, 'Microglia phagocytose stressed neurons resulting in delayed neuronal death by phagoptosis after brain ischaemia or inflammation', JOURNAL OF NEUROCHEMISTRY, Cairns, AUSTRALIA (2015) [E3] | ||||
| 2014 |
Fricker M, Walker MM, Talley NJ, Keely S, Hansbro P, 'Colon Pathology in a Mouse Model of Cigarette Smoke Induced Chronic Obstructive Pulmonary Disease (COPD) - A Model for Induction of Crohn's Disease?', GASTROENTEROLOGY, Chicago, IL (2014)
|
||||
| Show 29 more conferences | |||||
Grants and Funding
Summary
| Number of grants | 16 |
|---|---|
| Total funding | $2,006,346 |
Click on a grant title below to expand the full details for that specific grant.
20231 grants / $879,107
Further Understanding asThma REmission : The FUTURE research program$879,107
Funding body: GlaxoSmithKline (GSK) Research & Development Limited
| Funding body | GlaxoSmithKline (GSK) Research & Development Limited |
|---|---|
| Project Team | Doctor Michael Fricker, Conjoint Professor Peter Gibson, Professor Vanessa McDonald, Doctor Dennis Thomas, Doctor Rebecca McLoughlin |
| Scheme | Investigator Sponsored Studies |
| Role | Lead |
| Funding Start | 2023 |
| Funding Finish | 2026 |
| GNo | G2201070 |
| Type Of Funding | C3400 – International For Profit |
| Category | 3400 |
| UON | Y |
20201 grants / $766,205
Effect of mepolizumab on alternative functions of eosinophils in severe eosinophilic asthma – a prospective cohort study$766,205
Funding body: GlaxoSmithKline (GSK) Research & Development Limited
| Funding body | GlaxoSmithKline (GSK) Research & Development Limited |
|---|---|
| Project Team | Doctor Michael Fricker, Conjoint Professor Peter Gibson |
| Scheme | Supported Studies Programme |
| Role | Lead |
| Funding Start | 2020 |
| Funding Finish | 2023 |
| GNo | G1901465 |
| Type Of Funding | C3400 – International For Profit |
| Category | 3400 |
| UON | Y |
20186 grants / $257,034
Sputum mast cells as biomarkers of clinical phenotype and treatment response in COPD$60,000
Funding body: Thoracic Society of Australia and New Zealand
| Funding body | Thoracic Society of Australia and New Zealand |
|---|---|
| Project Team | Doctor Michael Fricker |
| Scheme | TSANZ/AstraZeneca - Respiratory Research Fellowship |
| Role | Lead |
| Funding Start | 2018 |
| Funding Finish | 2019 |
| GNo | G1800078 |
| Type Of Funding | C3200 – Aust Not-for Profit |
| Category | 3200 |
| UON | Y |
TSANZ / AstraZeneca Respiratory Research Fellowship$60,000
Funding body: The Thoracic Society of Australia and New Zealand
| Funding body | The Thoracic Society of Australia and New Zealand |
|---|---|
| Project Team | Michael Fricker |
| Scheme | Asthma and COPD Respiratory Research Fellowship |
| Role | Lead |
| Funding Start | 2018 |
| Funding Finish | 2019 |
| GNo | |
| Type Of Funding | Aust Competitive - Commonwealth |
| Category | 1CS |
| UON | N |
Protein Biomarkers in Asthma and COPD$52,034
Funding body: Phadia AB
| Funding body | Phadia AB |
|---|---|
| Project Team | Conjoint Professor Peter Gibson, Professor Vanessa McDonald, Doctor Michael Fricker |
| Scheme | Research Grant |
| Role | Investigator |
| Funding Start | 2018 |
| Funding Finish | 2018 |
| GNo | G1800031 |
| Type Of Funding | C3400 – International For Profit |
| Category | 3400 |
| UON | Y |
Priority Research Centre for Healthy Lungs Outstanding Scholar Award$45,000
Funding body: Priority Research Centre (PRC) for Healthy Lungs | The University of Newcastle
| Funding body | Priority Research Centre (PRC) for Healthy Lungs | The University of Newcastle |
|---|---|
| Project Team | Michael Fricker |
| Scheme | PRC Healthy Lungs Outstanding Scholar Award |
| Role | Lead |
| Funding Start | 2018 |
| Funding Finish | 2018 |
| GNo | |
| Type Of Funding | Internal |
| Category | INTE |
| UON | N |
Mast cell gene signatures for phenotyping in severe asthma$20,000
Funding body: Centre for Research Excellence in Severe Asthma
| Funding body | Centre for Research Excellence in Severe Asthma |
|---|---|
| Project Team | Michael Fricker, Peter Gibson, Vanessa McDonald, Natasha Winter |
| Scheme | NHMRC- Centre for Research Excellence in Severe Asthma |
| Role | Lead |
| Funding Start | 2018 |
| Funding Finish | 2019 |
| GNo | |
| Type Of Funding | External |
| Category | EXTE |
| UON | N |
Sputum columnar epithelial cells as biomarkers in severe asthma$20,000
Funding body: Centre for Research Excellence in Severe Asthma
| Funding body | Centre for Research Excellence in Severe Asthma |
|---|---|
| Project Team | Michael Fricker, Peter Gibson |
| Scheme | NHMRC- Centre for Research Excellence in Severe Asthma |
| Role | Lead |
| Funding Start | 2018 |
| Funding Finish | 2019 |
| GNo | |
| Type Of Funding | External |
| Category | EXTE |
| UON | N |
20173 grants / $47,000
Mast cell proteases as therapeutic targets for stroke$22,000
Funding body: Hunter Medical Research Institute
| Funding body | Hunter Medical Research Institute |
|---|---|
| Project Team | Doctor Michael Fricker, Professor Phil Hansbro, Professor Rohan Walker |
| Scheme | Project Grant |
| Role | Lead |
| Funding Start | 2017 |
| Funding Finish | 2017 |
| GNo | G1700861 |
| Type Of Funding | C3300 – Aust Philanthropy |
| Category | 3300 |
| UON | Y |
Macrophage dysfunction in severe asthma$20,000
Funding body: Centre for Research Excellence in Severe Asthma
| Funding body | Centre for Research Excellence in Severe Asthma |
|---|---|
| Project Team | Michael Fricker, Peter Gibson |
| Scheme | NHMRC- Centre for Research Excellence in Severe Asthma |
| Role | Lead |
| Funding Start | 2017 |
| Funding Finish | 2019 |
| GNo | |
| Type Of Funding | External |
| Category | EXTE |
| UON | N |
Utilisation of microbial products as novel therapies for COPD$5,000
Funding body: Hunter Medical Research Institute
| Funding body | Hunter Medical Research Institute |
|---|---|
| Project Team | Professor Phil Hansbro, Doctor Shaan Gellatly, Doctor Michael Fricker, Mr Kurtis Budden |
| Scheme | Greaves Family Postgraduate Top Up Scholarship in Medical Research |
| Role | Investigator |
| Funding Start | 2017 |
| Funding Finish | 2017 |
| GNo | G1700348 |
| Type Of Funding | C3300 – Aust Philanthropy |
| Category | 3300 |
| UON | Y |
20152 grants / $24,000
Determining the role of necroptosis in the pathogenesis of COPD.$22,000
Funding body: Rebecca L Cooper Medical Research Foundation Ltd
| Funding body | Rebecca L Cooper Medical Research Foundation Ltd |
|---|---|
| Project Team | Doctor Michael Fricker |
| Scheme | Research Grant |
| Role | Lead |
| Funding Start | 2015 |
| Funding Finish | 2015 |
| GNo | G1500294 |
| Type Of Funding | Grant - Aust Non Government |
| Category | 3AFG |
| UON | Y |
European Congress of Immunology, Austria 6-9 September$2,000
Funding body: University of Newcastle - Faculty of Health and Medicine
| Funding body | University of Newcastle - Faculty of Health and Medicine |
|---|---|
| Project Team | Doctor Michael Fricker |
| Scheme | Travel Grant |
| Role | Lead |
| Funding Start | 2015 |
| Funding Finish | 2015 |
| GNo | G1500927 |
| Type Of Funding | Internal |
| Category | INTE |
| UON | Y |
20131 grants / $20,000
DP73 Digital colour and monochrome camera + cellSens software + Xcite120 fluorescence lamp illuminator$20,000
Funding body: NHMRC (National Health & Medical Research Council)
| Funding body | NHMRC (National Health & Medical Research Council) |
|---|---|
| Project Team | Professor Paul Foster, Doctor Alan Hsu, Professor Phil Hansbro, Professor Joerg Mattes, Doctor Katie Baines, Professor Jodie Simpson, Professor Rakesh Kumar, Doctor Nicole Hansbro, Doctor Steven Maltby, Associate Professor Ming Yang, Doctor Gerard Kaiko, Professor Jay Horvat, Professor Simon Keely, Doctor Andrew Jarnicki, Doctor Michael Fricker |
| Scheme | Equipment Grant |
| Role | Investigator |
| Funding Start | 2013 |
| Funding Finish | 2013 |
| GNo | G1201186 |
| Type Of Funding | Other Public Sector - Commonwealth |
| Category | 2OPC |
| UON | Y |
20122 grants / $13,000
Elucidation of mechanisms of cachexia in COPD$10,000
Funding body: University of Newcastle
| Funding body | University of Newcastle |
|---|---|
| Project Team | Doctor Michael Fricker |
| Scheme | Early Career Researcher Grant |
| Role | Lead |
| Funding Start | 2012 |
| Funding Finish | 2012 |
| GNo | G1200889 |
| Type Of Funding | Internal |
| Category | INTE |
| UON | Y |
Investigating the role of MIC-1 in causing cachexia associated with chronic obstructive pulmonary disease$3,000
Funding body: University of Newcastle
| Funding body | University of Newcastle |
|---|---|
| Project Team | Doctor Michael Fricker |
| Scheme | New Staff Grant |
| Role | Lead |
| Funding Start | 2012 |
| Funding Finish | 2012 |
| GNo | G1200869 |
| Type Of Funding | Internal |
| Category | INTE |
| UON | Y |
Research Supervision
Number of supervisions
Past Supervision
| Year | Level of Study | Research Title | Program | Supervisor Type |
|---|---|---|---|---|
| 2022 | PhD | The Role of Fc Gamma Receptor and Fc Gamma Receptor-mediated Phagocytosis in Asthma | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2021 | PhD | Mechanisms and Therapeutic Targeting of Immunometabolism in Lung Disease | PhD (Immunology & Microbiol), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2021 | PhD | Investigating Aberrant Inflammatory Signalling in Asthma | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Principal Supervisor |
| 2021 | PhD | Characteristics of the Airway-Systemic Innate Inflammation Axis in COPD and Severe Asthma | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2020 | PhD | Characterisation of Neutrophil Subsets in Obstructive Airway Disease | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2020 | PhD | Utilisation of Diet and Microbial Products as Novel Therapies for COPD | PhD (Immunology & Microbiol), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2019 | PhD | Contribution of Cell Death to the Pathogenesis of Chronic Obstructive Pulmonary Disease (COPD) | PhD (Immunology & Microbiol), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2018 | PhD | Galectin-3 and Phagocyte Function in Asthma | PhD (Medicine), College of Health, Medicine and Wellbeing, The University of Newcastle | Co-Supervisor |
| 2016 | Honours | Altered macrophage signaling in COPD | Medical Science, The University of Newcastle - Faculty of Health and Medicine | Co-Supervisor |
| 2011 | Masters | CRT/LRP phagocytic signaling between microglia and neurons | Biochemistry & Cell Biology, University of Cambridge | Principal Supervisor |
Dr Michael Fricker
Position
Postdoctoral Research Fellow
School of Medicine and Public Health
College of Health, Medicine and Wellbeing
Contact Details
| michael.fricker@newcastle.edu.au | |
| Phone | (02) 4042 0207 |
Office
| Room | 2408 |
|---|---|
| Building | Hunter Medical Research Institute |

