University News
Menu
Modest, sustainable changes key to beating childhood obesity
An international study of weight management interventions for children above a healthy weight range or living with obesity has identified personalised, nutrition-led guidance is an effective strategy to achieve long term dietary changes.
Led by University of Newcastle Laureate Professor Clare Collins, the world-first systematic review of more than 100 dietary interventions for children and adolescents with obesity, investigated which approaches were most effective in improving dietary intake.
“The bottom line is, even modest changes, sustained over time, are important and improve diet, help create healthy eating patterns and improve nutrition-related health and well-being. People can stick with those changes,” Professor Collins said.
Childhood obesity remains a worldwide problem, with the global prevalence of children aged five to 19 who are above a healthy weight range, increasing from four per cent to 18 per cent between 1975 and 2016.
Modification of dietary intake is recommended as a key strategy to manage weight-related health in children.

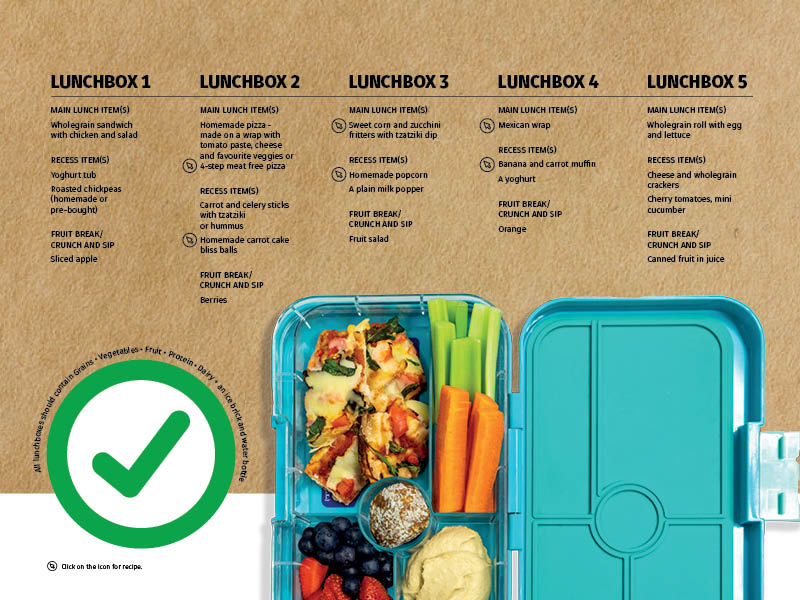
LUNCHBOX 1: MAIN LUNCH - wholegrain sandwich with chicken and salad RECESS - yoghurt tub, roasted chickpeas (homemade or pre-bought) FRUIT BREAK/CRUNCH AND SIP - sliced apple.

LUNCHBOX 2: MAIN LUNCH - homemade pizza - made on a wrap with tomato paste, cheese and favourite veggies or 4-step meat free pizza RECESS - carrot and celery sticks with tzatziki or hummus, homemade carrot cake bliss balls FRUIT BREAK/CRUNCH AND SIP - berries.

LUNCHBOX 3: MAIN LUNCH - sweet corn and zucchini fritters with tzatziki dip RECESS ITEM - homemade popcorn, a plain milk popper FRUIT BREAK/ CRUNCH AND SIP - fruit salad.

LUNCHBOX 4: MAIN LUNCH - Mexican wrap RECESS - banana and carrot muffin, a yoghurt FRUIT BREAK/ CRUNCH AND SIP - orange.

LUNCHBOX 5: MAIN LUNCH: wholegrain roll with egg and lettuce RECESS - cheese and wholegrain crackers, cherry tomatoes, mini cucumber FRUIT BREAK/CRUNCH AND SIP - canned fruit in juice.
The review assessed change in dietary intake by measuring key aspects of diet including total energy consumed, nutrients, food groups, diet quality and eating behaviour.
It found that obesity interventions incorporating a dietary component had a modest, yet sustained impact on reducing total energy intake and improving intakes of specific food groups in children and adolescents with obesity.
“Very few of these studies were designed to monitor dietary intake, and there is a tendency to only consider changes in body weight as outcomes,” Professor Collins said.
“If you take away all the bells and whistles suggested to families such as when to eat and when not to eat, the message is - if people work on reducing their total energy intake by changing the types and amount of foods selected, such as increasing their fruit and vegetable intake and cutting down on sweetened soft drink, it will have a positive impact.
“These messages seem obvious, but most interventions include a lot of other suggestions. People don’t need to do ‘fad diets’. Surprisingly, at a population level, it is unusual for people to actually eat enough fruit and vegetables.”
The current review identified dietitian-delivered, personally-tailored dietary advice for individuals and their families was an effective strategy to improve dietary compliance, optimise nutrient intake adequacy and achieve dietary intervention goals.
“This is the first time a systematic review of the nutritional messages has been undertaken – which messages are received, which messages are heard and are able to be implemented,” Professor Collins said.
The findings indicated that participation in moderate to high intensity interventions could result in short-term and longer term changes in total dietary intake and proportions of fat, protein and carbohydrate. However, severe nutrient restrictions, such as a very low carbohydrate intake, were not sustained.
“Food-based guidance, tailored for individuals and families, delivered by qualified dietitians, appears to be more effective in achieving longer-term dietary changes, rather than the provision of general dietary advice only,” Professor Collins said.
Six months post intervention, there was in general, a reduction in energy intake of about 800kj per day, which is equivalent to one to two serves of discretionary choices, or junk food. At the 12-month mark, the daily energy intake was still 500kj lower.
“Even if energy intake does not continue to decrease, small changes are enough to lower body weight over time,” Professor Collins said.
“It comes down to swapping something like a muesli bar for an apple, soft drink for water. The small changes add up.
“The message for families – what you put in the lunchbox or give for afternoon tea really matters.”
Professor Collins said health organisations and policy makers, including the World Health Organization, would find the data valuable to inform the development of evidence-based dietary guidelines for childhood obesity management.
Researchers from almost a dozen institutions contributed to the study, among them University of Hong Kong, the World Health Organization, University of New South Wales, Leeds Beckett University, the University of Queensland, Karolinska Institutet Sweden and The Children’s Hospital Westmead.
The study was partially funded through the Hunter Medical Research Institute (HMRI) and The Rainbow Foundation.
The paper, Impact of weight management nutrition interventions on dietary outcomes in children and adolescents with overweight or obesity: A systematic review with meta-analysis, was published in the Journal of Human Nutrition and Dietetics.
* HMRI is a partnership between the University of Newcastle, Hunter New England Health and the community.

Visit www.nomoneynotime.com.au for the recipes mentioned in this menu.
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.