Strengthening the defence against Leukaemia
Research from the University of Newcastle (UON) has revealed a more targeted way of treating T-cell acute lymphoblastic leukaemia (T-ALL), an aggressive type of cancer typically prevalent in children and adolescents.
The finding is an advancement in the field of biomedical science, and could provide patients with new treatment therapies that specifically target cancer cells and leave healthy cells intact.
UON’s senior author on the paper, Dr Matthew Dun, said the research could have an immediate impact on treatment strategies and change the way new treatment ideas are developed.
“This research has helped to provide some biological meaning to the cancer genome. We’ve been able to identify pathways that drive leukaemia, and then target these pathways with drugs that are clinically available. We hope that this precision treatment strategy will reduce long-term side effects and improve overall survival,” Dr Dun explained.
Children represent almost 60% of T-ALL cases. While survival rates are typically high, such intensive chemotherapy comes at the cost of significant short-term and potentially long-term side effects, including heart, lung, fertility and development problems.
Providing tumor-specific therapies will give children their best chance to develop into adulthood without damaging other cells or incurring secondary cancers.
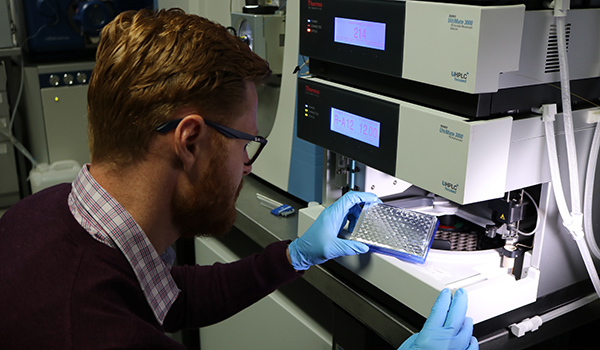
Dr Dun, also an affiliate of the Hunter Medical Research Institute (HMRI*), collaborated with researchers in Belgium to investigate a recurring gene mutation commonly found in cases of T-ALL through a process called protein sequencing.
“Cancer is a disruption to the genome – a combination of factors alter the genome, and these cause the cells to change into cancer cells. Proteins are the functional unit of every cell, with each cell containing up to a million or more different forms of protein.
“We specifically looked at a recurring gene mutation in T-cells that drives the development of ALL. This mutation causes the developing blood stem cells to stop maturing. Our capacity to perform deep sequencing allows us to dissect and identify proteins that drive leukaemia, enabling us to determine how the cancer cells are controlled by the mutated gene (JAK3).
“Our research is a step closer to investigating the drivers of all types of cancers, and developing cancer-specific targeted therapeutic strategies to reduce side effects and increase long-term survival. To reach this goal, we first need to understand the molecular mechanisms that underlie the leukaemia,” Dr Dun said.
Dr Dun collaborated with Belgium’s University of Leuven and the Leuven Cancer Centre on the study, which was published in the prestigious Leukemia journal.
* HMRI is a partnership between the University of Newcastle, Hunter New England Health and the community.
Related news
- Newcastle team on mission to improve childhood cancer outcomes
- Shanae’s passion for caring delivers her dream to work in health
- Food and nutrition degree serves Keren a rewarding career
- Kicking goals on and off the field, Joeli proves you can do it all
- Proving age is just a number, Arlyn wants to inspire more women in their 50s to pursue education
The University of Newcastle acknowledges the traditional custodians of the lands within our footprint areas: Awabakal, Darkinjung, Biripai, Worimi, Wonnarua, and Eora Nations. We also pay respect to the wisdom of our Elders past and present.